In the consulting work my partner Chunka Mui and I have done with senior management at major companies over the past dozen years, the most useful strategic planning tool we've developed is what we call a "future history." I'd like to try to apply that tool broadly, to the entire insurance industry. And I'd like your help.
A future history is a narrative written as though we're living five years, 10 years or even further in the future. A group -- usually a team of executives -- picks a point in time so it's close enough to today to be useful for planning purposes but far enough out that their thinking can go well beyond the three issues that most strategy discussions generally wind up focusing on: this quarter, next quarter and the quarter after that. The group then imagines what a perfect form of its business or industry might look like at that point in the future. This isn't done as an exercise in fantasy: The idealized form needs to be plausible based on trends in technology, in the economy in general, in behavior by customers and competitors, etc. Once the group narrows in on a plausible vision of nirvana, someone writes a "history" set on that date in the future that describes how the company or industry got there from here, as though it's already happened.
The future history not only gives executives unusual license to raise their sights but also gives them a story that organizes their thoughts and that they can easily remember and rally around -- one CEO, of a major insurance company, brought out his future history every year at his leadership meeting so they could track progress. Turning a vision into a narrative also can point out flaws in the logic -- "We need HOW big an increase in market share?"
Having published bits and pieces of a vision for the insurance industry for eight years now with ITL, I've taken the liberty of writing a future history for the insurance industry, set 10 years from now. I attach it at the end of this piece and very much hope you'll read it and react to it. You can reach me directly at paul@insurancethoughtleadership.com, or you can contribute to a public discussion at our page on LinkedIn. You can follow the discussion on LinkedIn; I'll also report back once the idea has taken more shape based on feedback.
First, some background on some general technology trends that I believe are in play, beyond what we're seeing about digitization, artificial intelligence and more in the day-to-day coverage of the insurance industry. Some of these may seem a bit far-out, but I assure you that I can back up what I'm about to say -- and, as I said, future histories are about really raising our sights and thinking big.
The trends are seven of what I call the Laws of Zero, which I've developed with Chunka and another longtime friend and colleague, Tim Andrews, in a book being published today. The book -- A Brief History of a Perfect Future: Inventing the World We Can Proudly Leave Our Kids by 2050 -- is set much further in the future than what I've written about insurance and focuses on how to tackle broad, societal issues such as healthcare, climate change and disinformation, but the Laws of Zero apply to all industries and will have major impact long before we hit 2050.
By a Law of Zero, we're referring to anything on an exponentially declining cost curve. When you look at that curve over a bit of time, the cost seems to be headed toward zero -- and anything that costs nothing is an infinitely(ish) available resource to throw at problems and opportunities.
Computing power is the area we're all most familiar with, because we've been experiencing the benefits of Moore's law ever since Intel co-founder Gordon Moore posited in the 1960s that the number of transistors on a computer chip (roughly a proxy for its processing power) would double every year for at least a decade. As those doublings have continued (sometimes faster, sometimes slower), we now have iPhones that would have been able to manage sending 120 million Apollo missions to the Moon and back -- at the same time. A gigabyte of memory cost more than $300,000 in the early 1980s; today, a gigabyte costs a fraction of a penny, and you'll soon be able to buy an iPhone with a terabyte of memory (1.024 gigabytes).
But that's all in the past. Now, as strategists, we need to imagine the future. What will computers, phones and other electronic devices look like in a decade when they are perhaps 30X to 50X as powerful as they are today, at no increase in cost? Surely, something new will arise for us as individuals, beyond texting and TikToks, but what will it be? And what new business models might become possible for insurers?
Computing is just the first Law of Zero. We also argue that communication will follow a Law of Zero (providing infinite(ish) bandwidth at zero(ish) marginal cost). Information will, too. The tiny satellites being launched by the dozens by SpaceX and others will blanket the globe with cameras and with communication capabilities, meaning everywhere will be within reach and can be monitored continually. Sensors and cameras, which just need a little solar power, a battery and a small antenna, will be capable of reporting from anywhere. Sensors on and even inside our bodies will let us and our doctors monitor our health in startling new ways.
Genomics is declining in cost and increasing in capability far faster than even Moore's law would suggest. Some 25 years ago, techniques would have required 86 million years to sequence an entire human genome. Today, that can be done overnight. And progress won't stop there, either -- an attachment is being developed for smartphones that will allow for sequencing a genome anywhere, any time, almost instantly. The implications go way beyond healthcare, too, reaching into almost every area related to biology.
We also posit Laws of Zero for energy, water and transportation. These are a bit squishier than those for computing, communication, information and genomics, but they're real and important.
Solar power costs, for instance, have already come down so fast that it provides the cheapest electricity. Soon, it will be cheaper to build new solar and wind capability than to buy coal and gas to fuel existing plants. Solar and wind will always carry a cost -- as will the batteries needed to store the power, and the reimagination of the grid that will have to occur to incorporate so much more renewable energy -- but carbon-free energy sources will be abundant and very cheap. So, people will be able to be profligate with their use, much as people now think nothing of using once-expensive bandwidth to watch football games on their phones.
Once energy becomes extraordinarily abundant and cheap, much of today's problems with water disappear. Some major cities, including Capetown, South Africa, have gone through water crises even though they sit cheek by jowl next to an ocean, but infinite(ish), carbon-free energy will make desalination feasible at scale. Some technologists have even made progress at using solar power to condense water out of the air and may be able to do that at enough scale to supply individual households -- as a demonstration, one company set up a water fountain in the middle of the Atacama Desert in Chile, the most arid spot in the world outside the polar deserts.
With transportation, even though autonomous vehicles will never be free -- they'll still need to be built and managed -- they will take away so many considerations of time and distance that they, too, can be seen as following a Law of Zero.
Some of these Laws of Zero are recursive. For instance, computing power has improved so much that it is enabling artificial intelligence that is designing specialized chips for AI, which will make it more powerful and let it design better chips... and so on. Many are mutually reinforcing: For instance, AI is allowing many genomic processes that used to be done in the lab to be done just as accurately on a computer, meaning that testing and progress can occur at the speed of silicon.
That's enough for now on the Laws of Zero. (If you want to read more, I'd encourage you to read this article that Chunka wrote for the International Insurance Society, a sister organization with ITL, or, of course, to grab the book, where we spend some 50 pages exploring the topic.)
The question now is: How do those Laws of Zero combine with other innovations in insurance to help us design a near-perfect form of insurance by 2031?
In another article for the IIS, Chunka suggests questions, including the following, to help guide our thinking on where to focus our innovation thinking:
- What are the most pressing protection gaps in the communities you serve? The candidate list is not short. Natural catastrophes like wildfires, heat waves, earthquakes, pandemics, flooding and other extreme weather events loom large. Long-term climate disruptions such as a rise in sea level, temperature shifts and droughts will be more severe. Additionally, technology-related risks like cybersecurity and large-scale technology failures could be more disruptive.
- How might those protection gaps evolve, especially for the most underserved?
- How might leading-edge tools enabled by the Laws of Zero be applied to better model risks?
- How might these tools transform every aspect of the insurance value chain, including product development, marketing and sales, underwriting and pricing, claims and customer service?
- How might early lessons from innovators and early adopters around the world be adapted to your community’s evolving challenges?
- How might your organization evolve to help markets and customers better understand their risk profiles and increase resilience, mitigate risk and reduce losses?
- How might your environmental, social, governance (ESG) strategy evolve, and what progress should be made in the allotted timeframe?
When I combined those questions with the capabilities of the Laws of Zero and other innovations, while trying to break free of the constraints we all know the industry faces and confront in our daily work, here is how I imagined an article on a near-perfect insurer appearing in a newspaper (electronically, of course) in 2031:
Insurer Sets Record for Market Value
PHILADELPHIA – Sept. 21, 2031 – The stock price of Transformative Insurance (better-known as TI) rose 3% today, making it the first insurance company to surpass $1 trillion in market value.
“They were the first in the insurance industry to figure out that nobody wants to buy insurance, while everybody wants to be safer,” said Steve Bern, a securities analyst at XYZ Research Corp. “For decades – actually, centuries – insurance promised people peace of mind and indemnified them after a loss. Well, nuts to that. Why not prevent that loss in the first place?”
Loss prevention has been the key at TI for a decade now. It basically aggregated the property/casualty industry’s data and sold services that helped car owners avoid accidents, let homeowners spot leaks before any damage could occur, warned business owners about situations that endangered employees and much more.
Sam Conroy, an analyst at ABC Consulting Group, said, “It wasn’t easy getting insurers to share their data. They aren’t known for sharing. But TI offered insurers a two-fer. Insurers would reduce the size and number of their claims by letting TI aggregate risk-related data, and – this was the big one – insurers got a chunk of equity in TI. TI basically operates as an industry consortium.”
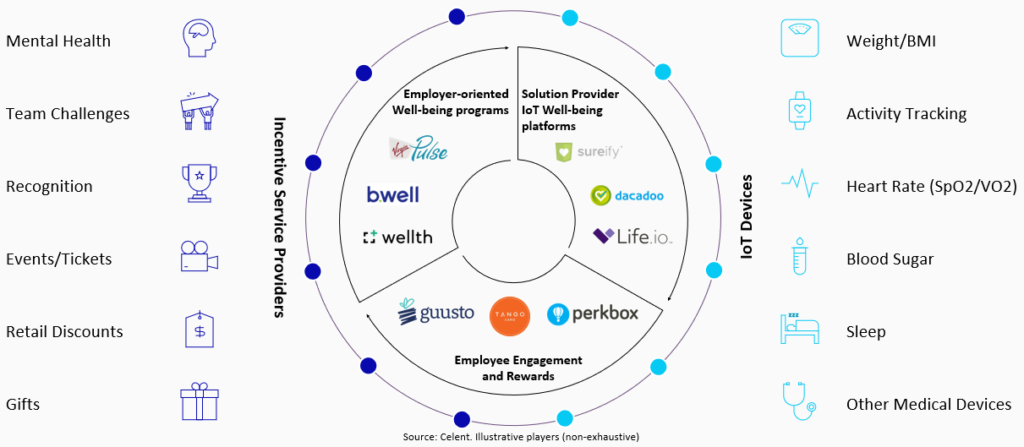
TI, in conjunction with all the major players in the insurance industry, has drawn on the Laws of Zero to deploy a wide array of technology in pursuit of risk reduction.
For instance, TI worked with auto insurers to spread technology pioneered by Nauto, which has tiny cameras mounted in the windshield that monitor both the road and the driver at the same time. These devices were initially deployed by fleet owners, who wanted to be able to check on drivers while going beyond measures such as hard braking – that hard brake might be a sign of inattention, or it might be a sign of an alert driver who saw a deer darting across a road. But the devices now do far more, because of the data and connections that TI provides.
The devices know where blind intersections and other trouble spots are, based on insurers’ accident data, and can warn drivers as they approach, especially if the camera shows the driver being inattentive. The devices now communicate with each other and can even create warnings in real time if a car up ahead hits an ice patch.
“Remember all those 30-car-and-truck pileups in the Tule fog in Sacramento in the winter?” Conroy asked. “No more. As soon as a crash happens, every car behind it gets warned to slow to a crawl and avoid the accident. Your car can now see around corners, too. No, it can't really, but a car around the corner from you can see that a car is about to run a red light or stop sign and instantaneously tell your car to halt until the bozo clears the intersection.”
TI also helped spread technology developed by Notion, which allowed for smart homes without all the installation costs that came with many early devices. The technology allows for a homeowner to place an inexpensive sensor (now costing only a few dollars) anywhere there might be a leak or at any door or window that the homeowner wants to monitor. The sensors communicate wirelessly with a hub in the house or apartment, which then connects with an app on the homeowners phone and, perhaps, with a professional service if the sensors are being used for home security.
“Uptake was swift for a reason that didn’t even occur to me,” Conroy said. “I figured people would like being able to spend a few dollars to prevent a potentially catastrophic leak, and they do, but they really liked that they could be notified when that front door opened and shut at 3:15, so they knew their kids were home safely from school. People wound up using these devices way more than they used any insurance app I’ve ever seen.”
TI has begun to expand into offering home maintenance advice – but very much as a trusted adviser and not, like some other companies, as a front for selling appliances or repair services. TI sensors monitor key pieces of equipment, such as a water heater, to watch for potential leaks. The company also recommends other home maintenance when it can present an argument that the homeowner will likely save money. In addition, TI has drones that can provide annual or semi-annual inspections that look for problems with gutters, roofs, etc., and has access to satellites that can monitor homes daily.
On the commercial side, TI offers a service that uses cameras -- now so cheap that they can be anywhere -- to evaluate workplaces for situations and practices that pose dangers to customers or employees, drawing on its definitive, continually updated data on previous claims. TI advises clients on how robots could take on dangerous tasks or can be used to make environments safer for customers – such as by using ultraviolet light to disinfect hotels or restaurants. In addition, TI steers clients toward exoskeletons that workers can wear to take over lifting tasks and prevent soft tissue injuries, which used to afflict so many workers.
“TI basically pulled off an Uber or an AirBnB,” said Debbie Colker, president of DEF Research Inc. “TI is a classic example of what Silicon Valley would call an ‘asset-light’ company. It doesn’t have to carry all the risk capital that the insurers and reinsurers have on their books. TI just manages the data and provides services that customers value very highly.”
TI’s success comes at a time when the entire industry is undergoing a technology-driven transformation that, among other things, has pushed operating costs down more than 50% in the past decade.
“I think the last fax machine just got crushed and dumped in a landfill,” Colker said.
Simply moving to a digital form of the business – accelerated greatly by the COVID-19 pandemic in 2020 and 2021 – took out much of the cost. Artificial intelligence, including robotic process automation, accomplished most of the rest. Blockchain contributed mightily, too, by providing an easy way to securely share masses of data that previously required waves of phone calls and emails.
"Lo and behold," Colker said, “making operations so much more efficient greatly narrowed the protection gap. Customers now get maybe 80 cents of each premium dollar back in a claim paid, rather than 60 cents, as they used to, because all those unnecessary costs are gone. Customers are still paying for peace of mind, but only about half as much as they did – now giving up only 20 cents of each premium dollar, rather than 40 cents. And they like that change. A lot.”
The transformation began in distribution but quickly moved into claims, then took over in underwriting – and now is cycling through the industry again.
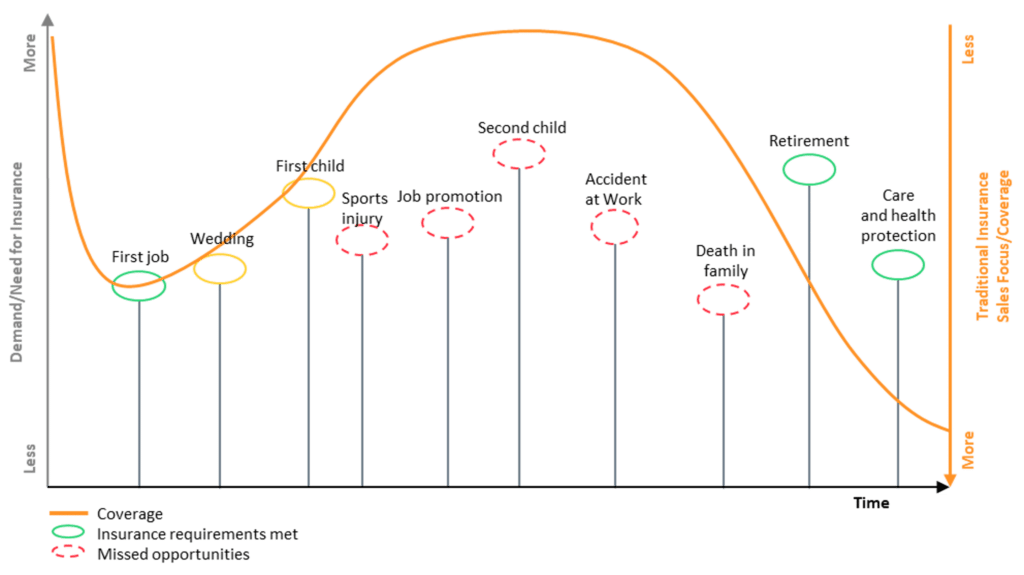
Simple digitization drove the initial change in distribution because it allowed for reaching customers in more efficient and even new ways – including through comparison sites, through social media and through platforms where brokers could place applications for insurance and have multiple insurers quickly bid on the business. Insurers could not only make their offerings more broadly available, far beyond the reach of a series of small offices in strip malls, but could allow customers to do research and begin the buying process online on their own – an especially important feature for younger prospects.
The pandemic in 2020 and 2021 accelerated the need for digital interactions, and the industry later settled into a hybrid, with digital increasingly carrying the load but human agents available whenever they were needed. Chatbots expanded the range of digital interactions, beginning by handling routine inquiries but gradually developing a more sophisticated range – again, always with human experts as a backstop. Robotic process automation now handles most of the coordination of the sales work, and e-signatures and e-payments removed a huge chunk of the paperwork. AI, meanwhile, makes agents much more accurate at identifying prospects.
The digital fervor spread soon enough to claims, where AI caused an even bigger change in the early 2020s than occurred with distribution. In the vernacular of the time, the claim became the boss of the process. Rather than think about a claim as a sort of folder passed down the line from person to person to person as it went from first notice of loss to payment, AI made the claim the central point and sent queries off to people and data bases – including a blockchain – as required to keep things moving along as quickly as possible.
The AI also continually sorted through claims in a sort of triage, paying some immediately because they seemed clean and because the cost of paying was lower than the cost of assigning an adjuster, while referring others to experts or fraud investigators. Parametric insurance, which is increasingly popular, requires that some claims be paid instantly, if, say, rainfall is below a certain level in a farming area.
“There was a lot of focus in the early 2020s about having AI generate an estimate on something like an auto claim, and that was certainly cool,” said Ruth Sze, the leader of the auto consulting practice at JKL Corp., “but the AI maybe saved an adjuster half an hour, and, truth be told, the estimates weren’t initially very accurate. Letting those involved in an accident take pictures shortened the process a lot more. And the really important change was putting the AI in charge; that cut many days out of an auto claim and slashed costs. In 2020, there were a billion days in the U.S. between when auto claims were filed and when they were paid. Now, we're down to single-digit millions.”
Underwriting came next. Based on the Laws of Zero for computing, communication and information, underwriters can now pull together information almost instantly, greatly accelerating the process, while AI has expanded access to lots of new sources, including unstructured information like photos and videos, as well as old, handwritten documents. Many types of commercial insurance can now even be initiated on a self-service basis by the customer, a la auto insurance starting in the 2010s. Customers can get an instant quote online and adjust coverages themselves to see the effect on price, before a broker gets involved to answer questions and review the coverage.
“Now the renewal process is starting back at distribution,” Sze said, “because the traditional part of the industry is finally stripped down to its digital essence. When you think of indemnification, there is a customer, a yes/no mechanism for deciding whether someone gets paid and, finally, capital. That’s it. Just those three elements.
“And now we’re free to pull capital from anywhere — insurers, reinsurers, the capital markets, wherever. We can have any kind of yes/no mechanism, whether that’s an adjuster, a parametric trigger or anything else. Distribution can be anything – and we’re seeing that. Traditional barriers are breaking down between, say, health and life insurance sales – both want to keep you healthy, right? Life insurance can be part of wealth management. Auto insurance can be sold along with an auto, home insurance along with a home. And so on.
“I’ve always thought the truest form of synergy was, ‘Do you want fries with that?’ Well, now everybody is asking on the industry’s behalf, ‘Do you want some insurance with that?’”
***
I realize this is far longer than my usual missives, but I didn't see any way to do this more succinctly. There's a lot going on here. I hope this stimulated your thinking and really do hope you'll either offer thoughts on how this hypothetical TI might be even better -- don't worry, I have a thick skin -- or suggest other avenues to pursue.
We have almost immeasurable capabilities that we can use to transform insurance, and, if we get the vision pretty much right, we can start planning now for 2031 rather than just waiting until we get there before really figuring out how to take advantage of what the Laws of Zero will deliver.
Cheers,
Paul