AI agents aren't just another layer of automation—they mark a fundamental shift in how insurers can scale decision-making and operations. Unlike traditional tools, they can interpret context, provide recommendations and carry out tasks across multiple systems. For insurers, this isn't about just answering questions—it means executing real work and driving measurable outcomes.
For example, an underwriter can ask an AI agent to review broker submissions, extract risk data and suggest pricing tiers based on historical patterns. A business analyst can use an AI agent to analyze customer lifetime value and identify new retention strategies. A product manager can even have an AI agent configure new insurance products based on specific business requirements. These agents accelerate operations and improve efficiency while leaving judgment and final decisions in human hands.
AI Experimentation Is Not Enough
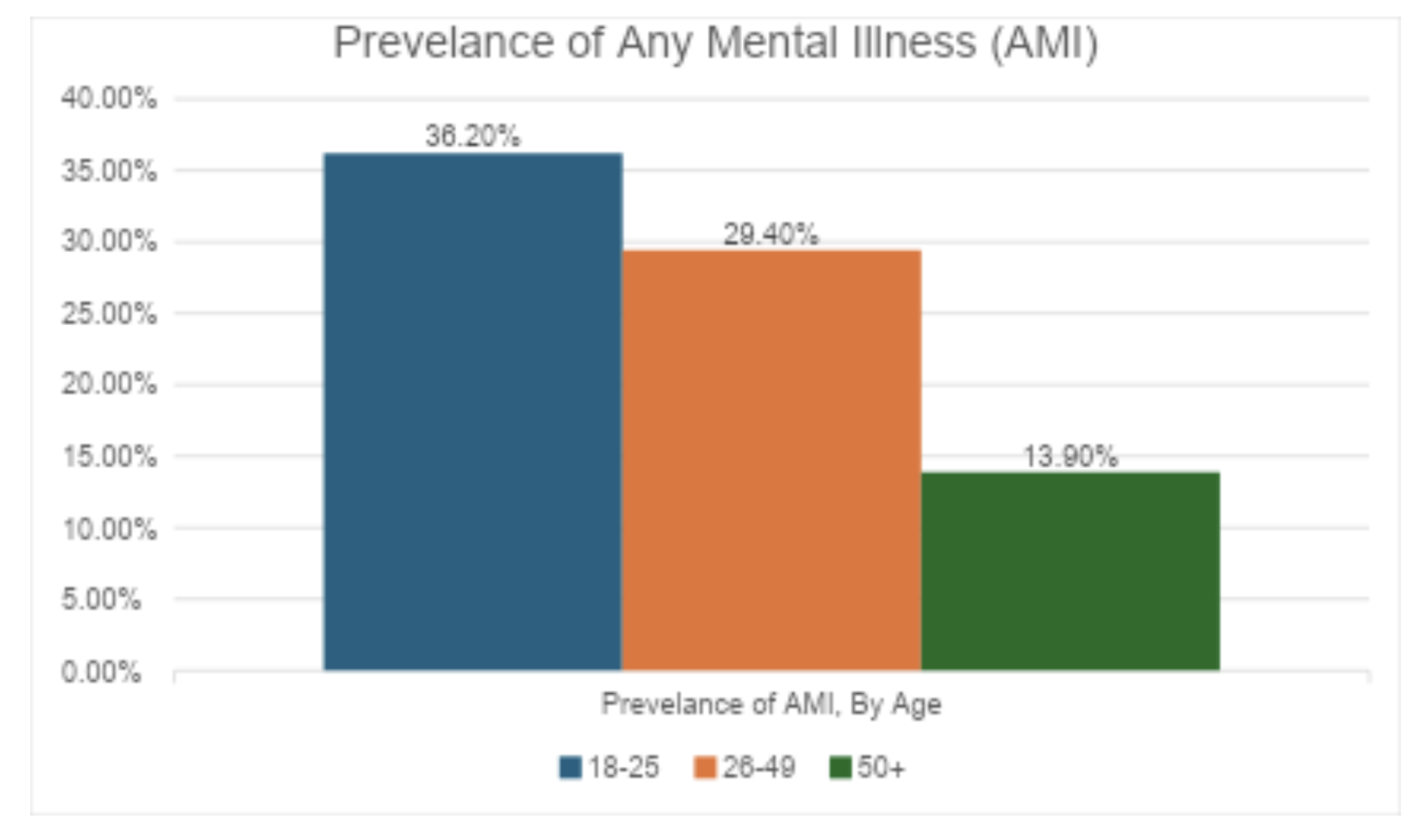
The potential is clear, but the reality is more complicated. According to Boston Consulting Group, 67% of insurers have experimented with AI, but only 7% have scaled it across their organizations. That means the vast majority remain in pilot mode, running isolated experiments that rarely expand into enterprise-wide capabilities.
That gap between promise and practice is where insurers risk falling behind. AI agents can deliver real value, but not if they remain trapped in proofs of concept. Scaling requires more than one-off pilots—it demands modern infrastructure, aligned leadership and interoperable systems that can evolve alongside the technology itself.
AI Agents Require Modern Infrastructure and Interoperability
Several technological obstacles keep insurers from deploying AI agents at scale. Legacy systems still dominate many organizations, making it difficult to connect AI to core functions like policy administration, billing and claims. Data is often fragmented, inconsistent and locked in silos, limiting the usefulness of even the most advanced models.
Even when insurers modernize their infrastructure, interoperability quickly becomes the new barrier. Today's AI ecosystem is highly fragmented, with each platform requiring custom development to connect with insurance workflows. The result is a patchwork of brittle integrations that are expensive to maintain and risky under real-world demands. Technical debt and compliance pressures only add to the complexity.
This creates vendor lock-in. Carriers often stay with a platform not because it's the best fit but because switching would mean rebuilding their entire AI infrastructure from scratch. The consequences are serious: Innovation slows, costs rise and insurers lose access to emerging capabilities that could deliver better results.
Enter the Model Context Protocol (MCP)
There have been several attempts to solve the AI interoperability challenge. Solutions like LangChain provided some help but locked organizations into specific frameworks, while function calling still required custom glue code for each connection. These early frameworks proved the demand for better connectivity but also exposed the limits of proprietary approaches.
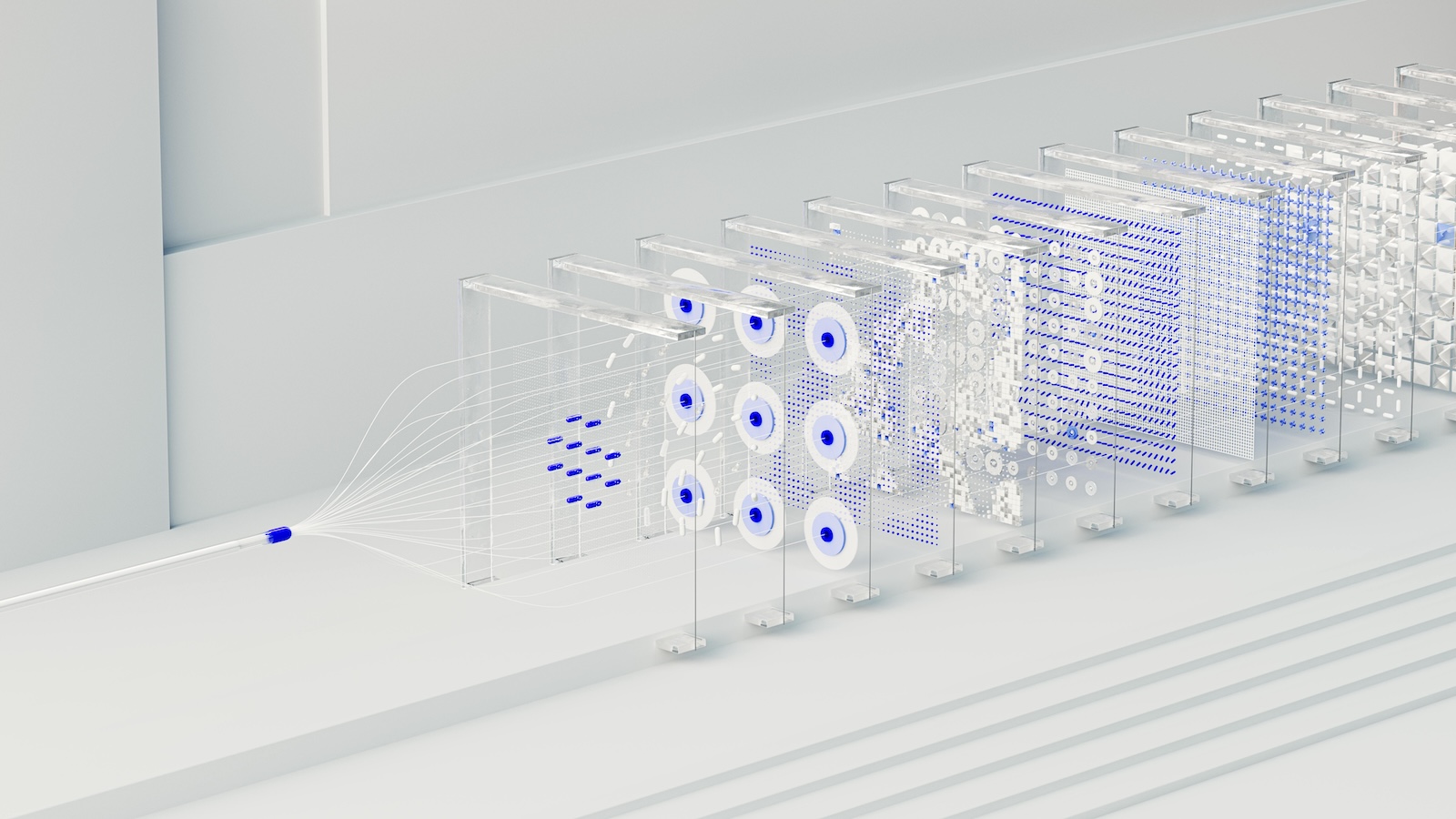
In contrast, the MCP, introduced in 2024 by Anthropic, establishes a universal, open protocol—similar to USB for hardware—that lets organizations write a connector once and use it across different AI models and providers. This standardization eliminates redundant work, enables clean separation between data sources and AI applications, and creates a true plug-and-play ecosystem for AI agent connectivity.
For the insurance industry, the implications are significant. MCP allows AI agents to execute workflows securely, with auditability and governance built in. It enables portability, so organizations can switch AI providers without rebuilding their integration layer. And it accelerates innovation, since new AI tools can be adopted faster and with less friction.
MCP isn't perfect, but it's the most widely adopted solution so far—and a major leap forward in enabling open, interoperable AI systems. That's why it has quickly gained traction among enterprise software leaders including Salesforce, Snowflake, Atlassian, Hubspot and many more.
How Core Platforms Can Deliver AI Connectivity
MCP solves the interoperability challenge, but it does not address the underlying data problem. AI agents are only as effective as the data they can access. If insurers rely on legacy systems with siloed or inconsistent data, even the most advanced AI deployments will underperform.
This is why insurers need modern core platforms built for data fluency—the ability to access accurate and complete data whenever it's needed, in whatever form the business requires. A data-fluent core platform provides:
- Cloud-native data availability and performance to support real-time workflows
- Flexible data access, such as open APIs, data lakes and event streams
- Complete and governed data with metadata, lineage and auditability for compliance
When paired with MCP, a data-fluent core creates the ideal foundation for agentic AI. It ensures that AI agents can connect seamlessly to critical workflows while reasoning across high-quality data. Together, they unlock not just isolated efficiency gains but the potential for enterprise-wide transformation.
The Path Forward
Even with interoperable systems and data-fluent cores, AI agents cannot operate in a vacuum. In a regulated industry like insurance, transparency and accountability remain nonnegotiable. Human-in-the-loop governance—reviewing recommendations, validating outputs, and ensuring fairness—will be essential to earning trust and meeting regulatory requirements.
The insurance industry has reached an inflection point. AI agents are powerful enough to reshape underwriting, analytics, and product design, but scaling them requires both standards like MCP and modern core systems designed for AI connectivity. By embracing open, interoperable architectures, insurers can avoid vendor lock-in, reduce complexity and accelerate innovation.
The winners will be those who understand that AI is not just about smarter models—it's about building the infrastructure that allows those models to thrive. With the right foundation in place, insurers can finally move beyond pilots and unlock AI as a true engine of innovation and growth.