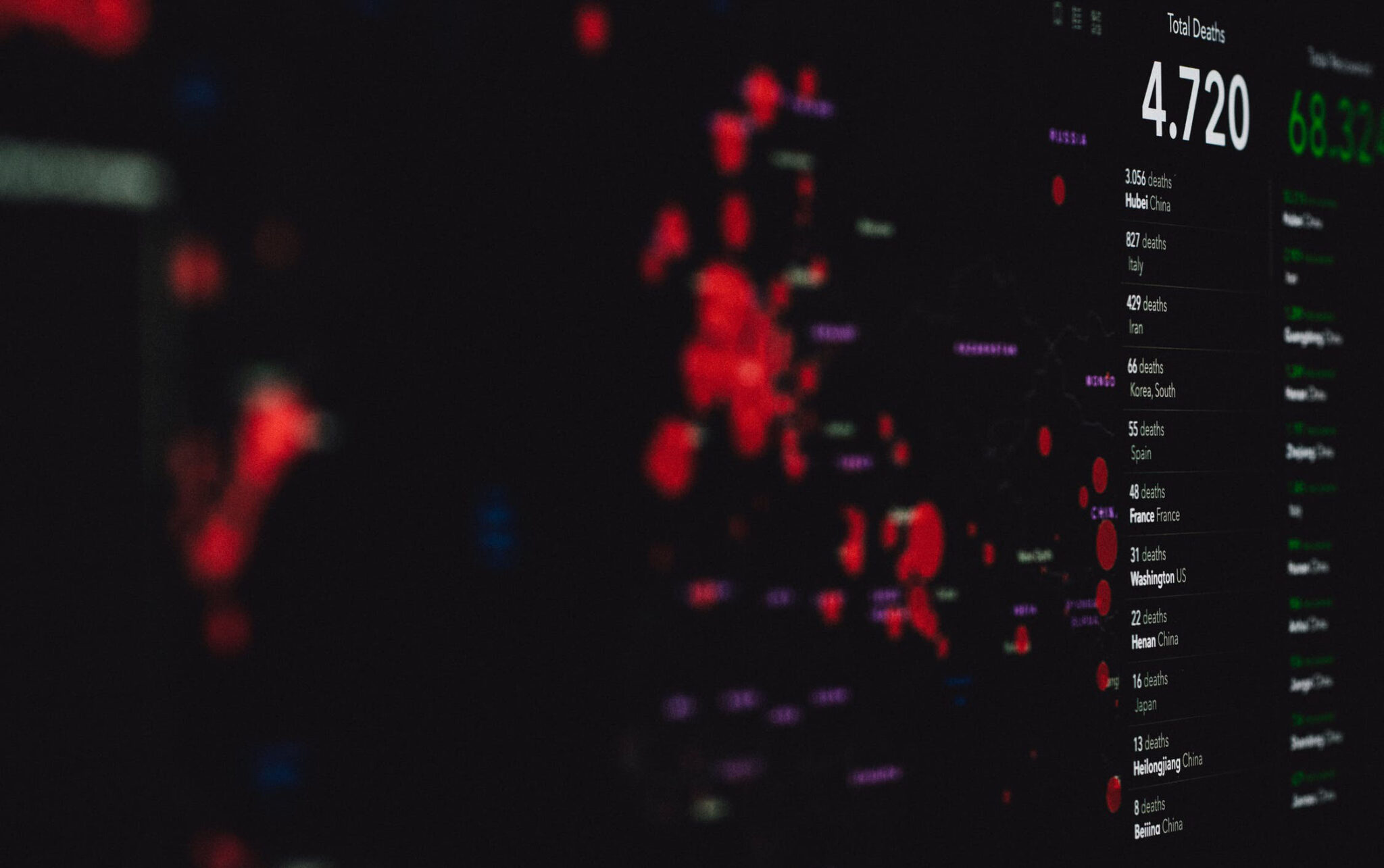
In 2020, catastrophic weather, including severe wildfires, seven major hurricanes and a destructive derecho drove the proportion of catastrophe losses up 40% from 2019. These weather events were the largest drivers of losses for the home insurance industry in 39% of claims – the highest percentage in the last six years, according to the new 2021 LexisNexis Home Trends Report.
Overall loss cost for all perils increased by 6% year-over-year, with some states more severely affected than others. Louisiana, for example, had the highest loss cost in the nation in 2020 due to a devastating hurricane season and overtook Colorado as the state most affected on average by wind peril in the last six years.
In the western part of the U.S., Colorado continues to rank highest in hail claims over states like Texas and Wyoming, while California accounted for the most loss cost, severity and frequency of fire and lightning claims, with 37% of all catastrophe claims nationwide and 75% of all catastrophe losses in 2020.
In addition to these extreme weather events, the report also tracked and analyzed the impact of COVID-19 on the U.S. home insurance market in 2020. Fewer houses were left unattended, with more people working from home, leading to a 53% decrease in liability and a 25% drop in theft loss costs.
As people go back to the office and school, it’s likely these perils will return to their respective longer-term trends, making it important for carriers to consider how to support homeowners in lowering their future risks.
To help carriers do that, the LexisNexis Home Trends Report provides by-peril home insurance data and location-based insights to help carriers make more informed risk assessments and underwriting decisions. Some of the additional key findings from the report by peril include:
Wind
- Wind frequency, loss cost and severity all increased significantly in 2020 – frequency increased by 42% this year and loss cost by 63%.
- 2020 marked the largest wind loss cost recorded in the last six years.
Hail
- Loss cost and severity of hail claims declined in 2020, while frequency remained steady.
- However, catastrophe claims made up 62% of all hail claims this year, and the frequency of hail catastrophe claims increased a significant 9.9% year-over-year.
- In 2020, catastrophe claims made up 62% of all hail claims – a marked increase compared with 2019, when just 56% of hail claims were catastrophe claims.
Fire and Lightning
- The 2020 wildfire season, the most active on record, led to increases beyond 2017 and 2018 levels in both loss cost and severity for insurers. The proportion of catastrophe losses also increased.
- Fire and lightning loss cost also increased year-over-year, having peaked in September following a dramatic uptick in frequency in August 2020.
Non-Weather-Related Water
- While the six-year trend for water claims not related to weather continued to climb, 2020 did see a decrease of 8.7% in loss cost compared with 2019 – likely a result of people spending more time at home and perhaps increased use of smart water leak detectors.
- Claim frequency decreased by 7.3% while severity remained steady.
See also: A Price Tag on Climate Change
For carriers looking to make location-based decisions, there are some additional state-specific key findings:
- Colorado and Nebraska ranked highest in loss cost over the six-year period from 2015 to 2020, while West Virginia and Maine ranked lowest.
- Likely as a result of Hurricanes Isaias, Marco and Laura hitting Louisiana and Texas, wind loss cost, frequency and severity all increased significantly in 2020. Loss cost rose 63%, and frequency increased 42% compared with 2019.
- Colorado ranked highest in loss cost over the six-year period from 2015-2020.
- California had the greatest non-weather-related water loss in 2020 at 100% higher than the national average loss cost.
With catastrophe claims driving losses and reinsurance costs higher, it's imperative for insurers to have the most recent peril-related trend data. Basing underwriting and pricing decisions on accurate and up-to-date data can help insurers meet loss-ratio objectives and growth targets, as well as support a better customer experience for consumers by helping homeowners avoid escalating costs.
These insights for both peril-related and location-based trends can help insurers assess and price risks more accurately, better assess their book of business and improve their understanding of how by-peril trends are changing over time. To download the full 2021 LexisNexis Home Trends Report, click here.