You can't be everywhere at once, and your training and processes can only be so good. Adjusters, especially junior adjusters, can miss things in claims files that make a big impact on losses. These might be big misses, like with deadlines, or might be smaller misses that have a big impact, like whether contributory negligence was present. Both these kinds of errors can have a significant impact on your bottom line.
Claim leakage can be avoided with better tools, and AI is the ideal solution. AI can handle most aspects of file review with accuracy and consistency. However, you need a trained AI model to yield true value.
If you already use a product like OpenAI's GPT, you know that it can run into issues with deep or complex issues. Even many of the newest models that help with deed research still run into problems with lengthy and detailed output at speed. However, you should not compare your experience with the publicly available models on the internet against the quality that AI-specific insurtech companies can provide. AI is amazingly accurate when properly directed and trained.
Well-trained AI can handle virtually all aspects of a file review. After a file is closed, AI can also supplement the audit process to ensure your carrier's best practices were followed. AI has the ability to review tens of thousands of pages and compare any checklist against the claim's ultimate outcome and payout. AI can be incredibly proficient at this kind of outcome.
Using AI does not mean you (or your team) abdicate control over claim files, or the review of files. You should still validate the data. However, because AI has the ability to cite to specific pages relevant to its analysis, this process can be significantly sped up. This is especially true with mountains of medical files that are not relevant to the claim, or significant witness statements or communication logs, where only small bits of information are helpful or relevant.
This kind of review catches mistakes quickly and can be a terrific learning tool for your team. AI can speed up training time for new adjusters, who can immediately see areas of files that they may have not considered. Even when adjusters are manually trained, AI can be implemented to validate results and facilitate faster understanding of the key job functions and key performance indicators.
AI is not perfect, but neither are humans. The good thing about programming AI is that it follows your instructions every time the same way. Even if some of its output needs adjusting here and there, AI can be given a checklist of 10, 20, or even 100 things to review for every single file. It can effectively replicate your best and brightest over and over again.
Replicating your "best" is a key point as you consider software options. You want an AI that will replicate the best practices in your organization that are followed by the top 1-5% of all adjusters (or whichever team you are considering the use of AI with). Good AI software will start with your output in mind and work backward to determine what data, and ultimately what type of AI focusing, is necessary to produce that best output.
This process is different from a technology company that wants reams of data to "find" and tell you about your company's best practices. This generally produces average results (at best) and requires substantial internal training and focusing time to get you something very useful. The process takes a very long time, does not succeed, and costs substantial amounts of money. The reason why this can fail is in the inherent nature of how AI learns.
If you give any AI system 100,000 documents and you ask it to provide you with key concepts from all those documents, it will do a good job at summarizing them. It may even produce parts of a usable document as a template. This is because AI works by looking for correlations in the content of the documents. It is going to look for the things that most commonly appear. If you think about all the sections within the 100,000 documents as appearing on a bell curve, AI is going to go for the meatiest middle part of that bell curve. It will give you the results that closely match the middle because it is looking for correlation among the documents.
The issue with AI giving you the meatiest middle part of the bell curve is that the middle is the average. Nobody wants the average. Mitigating risk and reducing losses isn't about catching the average issues within a file - it's about catching the absolute largest number of issues no matter who is reviewing the claim. Average seems helpful in theory but is a failure in practice.
You do not want AI to produce average results, so you do not want it to evaluate the middle section of the bell curve. You want it to give you the very best, which means you want the results from the right-most area of that bell curve that represents the top of the top results. Conversely, you want AI to stay away from the very worst examples that reside at the left-most area of the bell curve - the place where the majority of leakage resides.
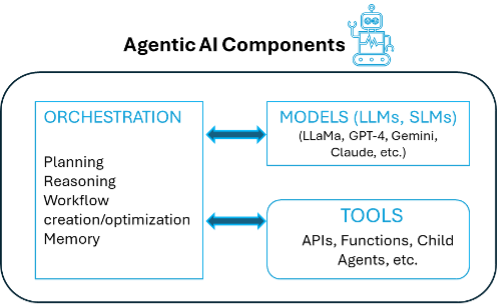
To get the best from AI, you must instruct it on your best practices. "Best practices" can mean either the best process/checklist you use, or the best example of a report that contains all the data you expect to see from your best people. Once you instruct AI on the best practices, then you can move backward into the reams of data to fill in the content. With the right application layer that directs AI, the results can be truly remarkable. This does not require creating a large language model just for your company's use, but rather harnessing smart applications built on top of the existing models.
Remarkable results can help reduce risk through better and more consistent file analysis, whether by an adjuster, outside counsel, or as part of a file audit. It can also reduce staff time by removing much of the labor-intense review of files that can take hours or days. Because AI doesn't get hungry, stressed, or tired, the time savings also means higher quality.
AI can offer greater benefits beyond time and file management. For example, AI can identify red flags in files, like excessive treatment, pre-existing conditions, or missing documents. It can provide an adjuster with a clearer understanding of property damage or bodily injury to better assess the claimant's demand. Using AI can even reduce the likelihood of a claimant getting counsel because an offer can be made within days versus weeks of the first notice of loss. The faster an offer is made, the less likely the claimant is to hire a lawyer.
Addressing demand letters is a new and powerful use of AI that smart carriers are implementing immediately. The plaintiffs' bar is already using AI to produce those demand letters, and the companies creating them brag about how much more money their AI-generated demands yield. One demand-generating company that recently raised funds on a billion-dollar valuation advertises that its users are 69% more likely to max out policy limits.
AI can effectively be used to counter these demands by recognizing holes in the file and presenting those to claimant's counsel. This includes identifying holes in coverage, such as endorsements or intentional conduct that might reduce or eliminate exposure. AI can do an initial review of liability by comparing police reports and witness statements to determine causation, and even flag contributory negligence and the lack of mitigation of damages.
As part of a file review, AI can also analyze damages and whether those appear excessive in light of the injury or economic information in the file. These kinds of robust demand responses point out all the ways a claim's value is not as high as the other side believes. This can yield higher leverage and lower payouts through appropriate risk analysis. This kind of analysis and response would be ideal for every file, but it takes a lot of time to do manually. AI offers the ideal solution, with the ability to produce a comprehensive response in less than five minutes.
AI can also reduce employee and customer churn. Using AI can lead to greater job satisfaction for adjusters and for customers. Your employees all of a sudden get to focus most of their time on the things that bring purpose and meaning to their jobs. They get to think more about strategy, talking to stakeholders, and analyzing files versus simply sifting through piles of documents that AI can do faster and more accurately anyway.
Customers are less likely to churn as claims are resolved faster and at fairer, more consistent valuations. When AI follows the same standards in every file, then variation in claim payouts stabilize, leading customers to appreciate the transparency and speed in which their claim is resolved.
The benefits of using AI are many, but it is not perfect. However, when AI reduces the time and energy it takes to review one file from 20 hours to two, that still equals a savings of 18 hours. And that is just one file. As you consider using AI for your organization, focus first on the best results that your best people produce. Then work backward. Also remember that perfect should not be the enemy of the good.