Handling Transition to a Public Company
The transition for a private company going through an IPO can bring unwelcome surprises, including with its D&O insurance.

The transition for a private company going through an IPO can bring unwelcome surprises, including with its D&O insurance.

Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|

Chris Rafferty is the chief operating officer of Aon’s financial services group (FSG). He is responsible for serving some of Aon’s largest FSG clients, as well as operational strategy, collaboration and best practices across FSG’s specialties and adjacent financial lines.
While proposals are well-automated, and so is policy administration, between the two comes group onboarding. It's a mess.

Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|

Jeffrey M. Weaver, FLMI, is director of underwriting and actuarial services at Global IQX, a provider of software to group benefits insurers.
Will the future of driverless cars fulfill its grand promise -- or rhyme with the history of the Segway?

Will the future of driverless cars rhyme with the history of the Segway? The Segway personal transporter was also predicted to revolutionize transportation. Steve Jobs gushed that cities would be redesigned around the device. John Doerr said it would be bigger than the internet. The Segway worked technically but never lived up to its backers’ outsized hopes for market impact. Instead, the Segway was relegated to narrow market niches, like ferrying security guards, warehouse workers and sightseeing tours.
One could well imagine such a fate for driverless cars (a.k.a. AVs, for autonomous vehicles). The technology could work brilliantly and yet get relegated to narrow market niches, like predefined shuttle routes and slow-moving delivery drones. Some narrow applications, like interstate highway portions of long-haul trucking, could be extremely valuable but nowhere near the atmospheric potential imagined by many—include me, as I described, for example, in “Google’s Driverless Car Is Worth Trillions.” For AVs to revolutionize transportation, they must reach a high level of industrialization and adoption. They must enable, as a first step, robust, relatively inexpensive Uber-like services in urban and suburban areas. (The industry is coalescing around calling these types of services “transportation as a service,” or TaaS.) In the longer term, AVs must be robust enough to allow for personal ownership and challenge the pervasiveness of personally owned, human-driven cars. See also: Where Are Driverless Cars Taking Industry? This disruptive potential (and therefore enormous value) is motivating hundreds of companies around the world, including some of the biggest and wealthiest, such as Alphabet, Apple, General Motors, Ford, Toyota and SoftBank, to invest many billions of dollars into developing AVs. The work is progressing, with some companies (and regulators) believing that their AVs are “good enough” for pilot testing of commercial AV TaaS services with real customers on public roads in multiple markets, including Singapore, Phoenix and Quangzhou. Will AVs turn out to be revolutionary? What factors might cause them to go the way of the Segway—and derail the hopes (and enormous investments) of those chasing after the bigger prize? Getting AVs to work well enough is, of course, a non-negotiable prerequisite for future success. It is absolutely necessary but far from sufficient. In this three-part series, I look beyond the questions of technical feasibility to explore other significant hurdles to the industrialization of AVs. These hurdles fall into four categories: scaling, trust, market viability and secondary effects. Scaling. Building and proving an AV is a big first step. Scaling it into a fleet-based TaaS business operation is an even bigger step. Here are seven giant hurdles to industrialization related to scaling:
Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|
Chunka Mui is the co-author of the best-selling Unleashing the Killer App: Digital Strategies for Market Dominance, which in 2005 the Wall Street Journal named one of the five best books on business and the Internet. He also cowrote Billion Dollar Lessons: What You Can Learn from the Most Inexcusable Business Failures of the Last 25 Years and A Brief History of a Perfect Future: Inventing the World We Can Proudly Leave Our Kids by 2050.
A hair-raising drive from Kathmandu to the Nepalese town of Hetuada provides the lessons of entrepreneurship in microcosm.

Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|

Bobbie Shrivastav is founder and managing principal of Solvrays.
Previously, she was co-founder and CEO of Docsmore, where she introduced an interactive, workflow-driven document management solution to optimize operations. She then co-founded Benekiva, where, as COO, she spearheaded initiatives to improve efficiency and customer engagement in life insurance.
She co-hosts the Insurance Sync podcast with Laurel Jordan, where they explore industry trends and innovations. She is co-author of the book series "Momentum: Makers and Builders" with Renu Ann Joseph.

Eighty years after Karen Blixen published her memoir, "Out of Africa," it may be time for the local insurance industry to start writing a sequel: "Into Africa."
That thought is prompted by a seminar that Africa Re hosted last week in Lagos, Nigeria, and that was put on by our chief innovation officer, Guy Fraker, and by our friend Grace Vandecruze, a veteran investment banker who is now the managing director of Grace Global Capital. Several dozen executives attended from the biggest insurers in Nigeria and Ghana, underscoring the interest in innovation among companies operating on a continent with almost unimaginable opportunity.
Grace said South Africa is the only country on the continent with any significant penetration by insurance products, and just 17% of households there own at least one insurance policy. In every other African country, she said, market penetration ranges from a fraction of a percent to a mere 4% of households. Meanwhile, the continent is home to more than 1.2 billion people and has six of the 10 fastest-growing economies in the world.
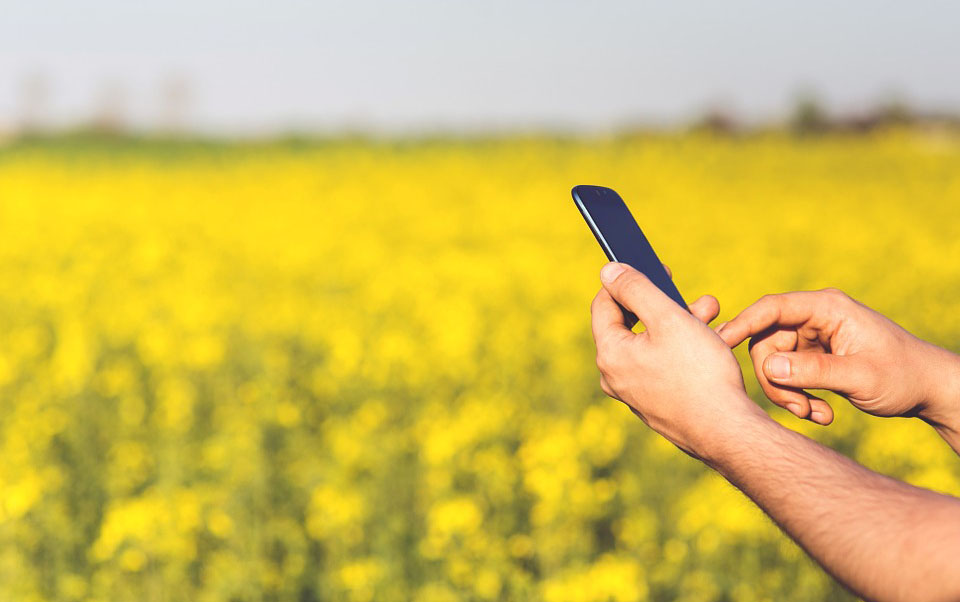
Virtually everyone on the continent has a cellphone, so, while companies in the U.S. and Europe complain about having to adapt legacy distribution and customer service networks to the demands of digital customers, insurers in Africa can develop optimized, fully digital systems from the get-go. African countries may also be able to leapfrog more-developed economies and build telecommunications systems based on the next generation of wireless technology, which is known as 5G and which promises Wi-Fi-like capabilities everywhere (though the jury is still out on the actual capabilities of 5G).
When I covered the computer industry for the Wall Street Journal in the '80s and '90s, a common geek joke was:
Q: "How did God manage to create the world in only six days?"
A: "He didn't have an installed base."
Ba-dum-bum.
But the punchline applies here: Because Africa doesn't have an installed based in insurance or in many of the underlying technologies that are being deployed by the industry in other parts of the world, insurers there have a chance to do things right the first time and leapfrog the rest of the globe.
I'm not suggesting that hundreds of business development types from outside the continent immediately book flights to Lagos and other African business centers. There is considerable expertise already there among the major insurers, sometimes facilitated by our new friends at Africa Re.
Insurance still needs to establish a trust factor among consumers in Africa, but the good news, Guy says, is that the low penetration of insurance means that companies have a unique opportunity to work together as a community for now, rather than as competitors. Basically, you have to have a pie before you start fighting over how to divvy it up.
So, let's all do all we can to help bake that pie. As we all know, broadly available insurance will provide stability that the people in Africa and their economies can build on.
Have a great week.
Paul Carroll
Editor in Chief
Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|

Paul Carroll is the editor-in-chief of Insurance Thought Leadership.
He is also co-author of A Brief History of a Perfect Future: Inventing the Future We Can Proudly Leave Our Kids by 2050 and Billion Dollar Lessons: What You Can Learn From the Most Inexcusable Business Failures of the Last 25 Years and the author of a best-seller on IBM, published in 1993.
Carroll spent 17 years at the Wall Street Journal as an editor and reporter; he was nominated twice for the Pulitzer Prize. He later was a finalist for a National Magazine Award.
The insurance industry has largely resisted, but companies that aren’t racing to innovate will soon be left behind.

Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|

Haywood Marsh is general manager of NetClaim, which offers customizable insurance claims reporting and distribution management solutions. He leverages experience in operations, marketing, strategic planning, product management and sales to drive the execution of NetClaim’s strategy.
Data prefill has reached commercial lines: Businesses need a simpler application, and distributors need to be freed from clerical tasks.

Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|

Karen Pauli is a former principal at SMA. She has comprehensive knowledge about how technology can drive improved results, innovation and transformation. She has worked with insurers and technology providers to reimagine processes and procedures to change business outcomes and support evolving business models.
Insurance companies must attack financial crimes or they may be next, after banks, to receive the attention of examiners.

Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|

Edmund Tribue is the risk and regulatory practice leader for NTT DATA services.
While there is an almost endless selection of service offerings available to agencies, a select few – like workflow management – are crucial.
Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|
Large books of low-volatility policies, normally covered by primary insurers, could be packaged by others into securitized risk pools.

Get Involved
Our authors are what set Insurance Thought Leadership apart.
|
Partner with us
We’d love to talk to you about how we can improve your marketing ROI.
|

Donna Galer is a consultant, author and lecturer.
She has written three books on ERM: Enterprise Risk Management – Straight To The Point, Enterprise Risk Management – Straight To The Value and Enterprise Risk Management – Straight Talk For Nonprofits, with co-author Al Decker. She is an active contributor to the Insurance Thought Leadership website and other industry publications. In addition, she has given presentations at RIMS, CPCU, PCI (now APCIA) and university events.
Currently, she is an independent consultant on ERM, ESG and strategic planning. She was recently a senior adviser at Hanover Stone Solutions. She served as the chairwoman of the Spencer Educational Foundation from 2006-2010. From 1989 to 2006, she was with Zurich Insurance Group, where she held many positions both in the U.S. and in Switzerland, including: EVP corporate development, global head of investor relations, EVP compliance and governance and regional manager for North America. Her last position at Zurich was executive vice president and chief administrative officer for Zurich’s world-wide general insurance business ($36 Billion GWP), with responsibility for strategic planning and other areas. She began her insurance career at Crum & Forster Insurance.
She has served on numerous industry and academic boards. Among these are: NC State’s Poole School of Business’ Enterprise Risk Management’s Advisory Board, Illinois State University’s Katie School of Insurance, Spencer Educational Foundation. She won “The Editor’s Choice Award” from the Society of Financial Examiners in 2017 for her co-written articles on KRIs/KPIs and related subjects. She was named among the “Top 100 Insurance Women” by Business Insurance in 2000.