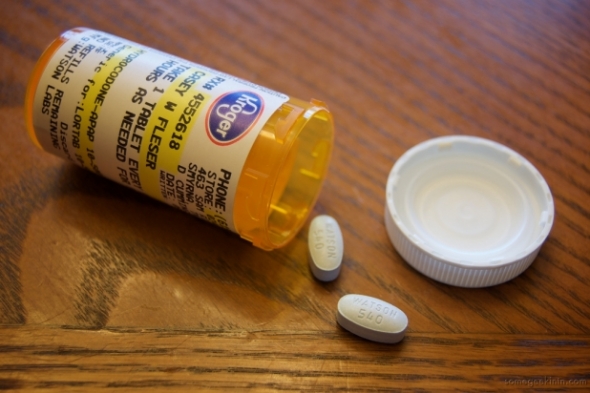
At a cost of more than $1.4 billion annually, narcotics and opioids have rapidly become one of the highest-cost therapeutic categories for workers’ compensation injuries.* They are also among the most difficult to manage. No employer wants to have injured workers in undue pain or discomfort – and narcotics do alleviate pain. However, there are serious issues to consider with regard to prescription abuse and misuse, especially for opioids such as Oxycontin and Vicodin.
How can employers help injured workers while ensuring appropriate use of narcotics and reducing unnecessary costs? Comprehensive, clinically based narcotic management programs can help.
Over the past 10 years, opioids, a type of narcotic, have become more commonly used to treat chronic to severe pain associated with workers’ compensation injuries. Known by the generic names of morphine or codeine, and now more frequently by the brand names Oxycontin and Vicodin, opioids are powerful pain relievers.
However, many of these medications were initially intended for end-stage cancer, not for common workplace injuries. While there is likely some benefit in some cases for the use of such medications to treat workers’ compensation injuries, clinicians note that those benefits are typically seen by just a small percentage of patients. There is little evidence to support their long-term or widespread use in standard workers’ compensation injuries. In fact, a study reported by the American Insurance Association found that only a minority of workers with back injuries improved their level of pain (26%) and function (16%) with the use of opioids.** What’s more, there is a high risk for abuse, dependency, and overutilization with this classification of drugs. Indeed, the strongest predictor of long-term opioid use was when it was prescribed within the first 90 days post-injury; that means that every prescription – especially the first one – must be scrutinized to ensure appropriate utilization and optimal benefit. Employers are also concerned about the cost of narcotics. While narcotic use is concentrated among a small percentage of claimants, per-claim costs for narcotics have increased more than 50% over the past decade
Key statistics
- From 1997 to 2007, the milligram per person use of prescription opioids in the U.S. increased from 74 milligrams to 369 milligrams – that’s an increase of 400%.
- In 2000, retail pharmacies dispensed 174 million prescriptions for opioids; by 2009, 257 million prescriptions were dispensed – an increase of more than 40%.
- Opioid overdoses, once almost always because of heroin use, are now increasing because of abuse of prescription painkillers.
White House Office of National Drug Control Policy
Managing narcotics is not about removing viable medications for mitigating pain from the therapies available to providers – it is about ensuring the best possible medications for workers’ compensation injuries are used.
As a result, claims examiners should be trained to look for red flags, such as:
- Higher-than-normal physician dispensing.
- Lower-than-average generic dispensing.
- Higher-than-average prescribing of opioids such as Fentanyl Citrate.
But prescribing medications is a complex issue – reports and percentages alone don’t tell the whole story. So, it’s crucial to look beyond simple prescribing reports to uncover additional information that could indicate why prescribers’ patterns are outside the norm. For example, use of amphetamines could indicate that a patient has a traumatic brain injury, where such medications are a standard treatment protocol.
Drugs that are not suitable for the injury type and the age of the claim need to be identified at the point-of-sale, so claims examiners or nurses are alerted before a prescription that is outside the formulary is filled at the retail pharmacy and can intercede with drug management, if needed. This is particularly useful in the acute injury stage to eliminate early narcotic use where it is not appropriate. If a narcotic is prescribed, the injured worker’s entire medical history needs to be reviewed, using both in-network and out-of-network transactions and non-occupational associated medications to evaluate actual medication use and ensure appropriate utilization.
Follow-up appointments should be required, and only a few days of treatment should be authorized initially. This helps determine whether the medication has improved pain control and function.
Another critical step to managing narcotics is to thoroughly educate employees as to the benefits, dangers, and alternatives for narcotics. The education should include:
- Training the injured workers about their medication, adverse side effects, and alternative medication options.
- Required screenings for risk of addiction or abuse (history of drug or alcohol abuse, or regular use of sedatives).
- Opioid use agreement/contract with urine drug screenings and avoidance of other sources for medication, such as emergency rooms.
A number of factors should trigger a review:
- Narcotic-class medications for the treatment of pain (Oxycontin, Demerol, etc.).
- Use of multiple medications excessively or from multiple therapeutic classes.
- Using medications not typical for the treatment of workers’ compensation injuries.
- High-cost medications.
- Receiving high doses of morphine equivalents daily for treatment of chronic pain.
- Using three or more narcotic analgesics.
- Receiving duplicate therapy with NSAIDs, muscle relaxants or sedatives.
- Using both sedatives and stimulants concurrently.
- Using compounded medications instead of commercially available products.
* “Narcotics in Workers Compensation,” NCCI Research Brief, Dec. 2009
** http://www.aiadc.org/AIAdotNET/docHandler.aspx?DocID=351901