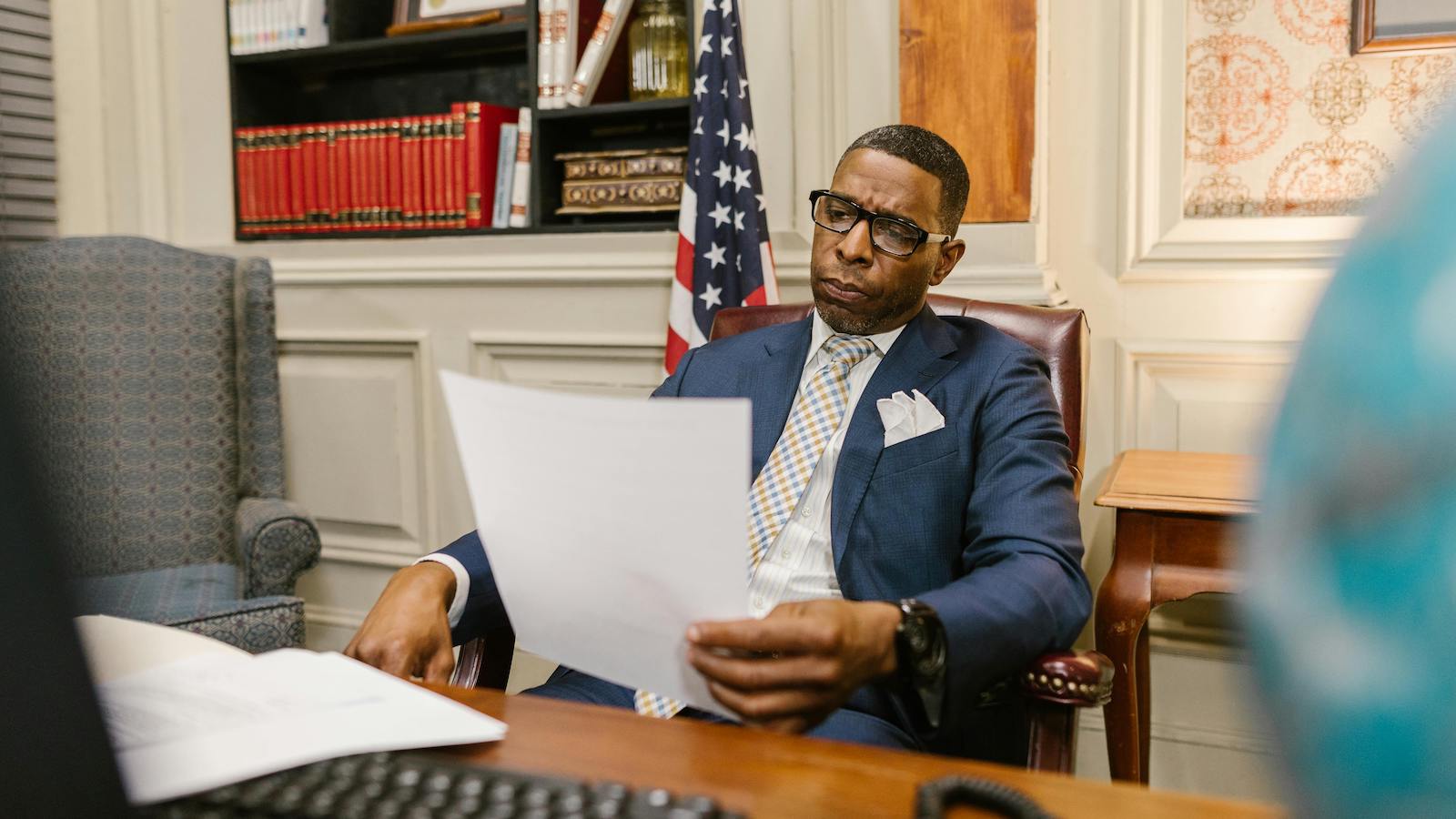
Behind every false claim is a carefully crafted narrative to deceive insurance companies. Fabricated accidents, exaggerated injuries, and staged losses are all framed within seemingly real paperwork. Not only is this an issue for insurers, but policyholders equally bear the brunt of paying for the losses through higher premiums.
An estimated 20% of insurance claims are fraudulent. Even more surprising is that an estimated $308.6 billion is lost to insurance fraud annually in the U.S. alone, costing an estimated $900 per policyholder. Imagine the losses insurers and policyholders bear in the rest of the world. The figure will certainly be jaw-dropping!
But what leads to such a high rate of insurance fraud? Scammers take advantage of the fundamental limitations of traditional fraud detection systems, which is their inability to understand human language. Thus, this has become the new focus in insurance fraud prevention, where the line between genuine and false claims often lies in the subtle details of written text.
There's an urgent need for insurance policy administration systems augmented with natural language processing (NLP) capabilities. These advanced systems can analyze huge amounts of unstructured data quickly and accurately. The result? More effective fraud detection and prevention without compromising the legitimate customer experience.
Before diving into the powerful capabilities and benefits of NLP-powered policy administration systems, it is important to understand why traditional systems fail today. So, let's get started.
Why Traditional Policy Administration Systems Fall Short
Traditional fraud detection systems have rule-based, static algorithms that struggle to detect advanced fraud strategies today. These outdated systems create significant vulnerabilities within insurance operations, leading to serious compliance issues and substantial financial losses. Take a closer look at the limitations of traditional systems:
1. Limited Fraud Detection Abilities
The legacy policy administration system in insurance has limited fraud detection capabilities and struggles to identify subtle patterns that might indicate fraudulent behavior. Moreover, the manual review process creates unnecessary bottlenecks and delays claim settlements. When suspicious activities trigger alerts, investigators often have to dig through documents, slowing the entire claims process for all policyholders.
2. Inability to Process Unstructured Data
Important information often lies in unstructured formats, such as adjuster notes, medical reports, and customer communication. Traditional solutions can't interpret these descriptions, given their inability to extract and process unstructured data. This creates significant blind spots in fraud detection efforts, as important red flags remain hidden within claim details, medical notes, and policyholder communication.
3. Reactive Rather Than Proactive
Legacy policy administration systems identify fraud during post-payment audits. More concerning is that these systems aren't connected to data sources; thus, they fail to capture valuable context that could reveal suspicious patterns. This reactive approach drains substantial funds way before fraud is even detected. Besides, recovery efforts prove costly and often unsuccessful compared to prevention strategies.
4. Inflexible Rules and Parameters
Traditional policy administration solutions require manual reprogramming to adapt to modern fraud techniques. Insurers require technical expertise for this process, which creates operational delays and downtime. Fraudsters know how to exploit the static thresholds built into traditional systems.
Not only this, but fixed threshold parameters trigger excessive false alarms that drain investigative resources, failing to identify advanced fraud attempts that circumvent predefined rules. The rigidity of these systems prevents the continuous improvement necessary to fight evolving fraud strategies.
As is evident, insurers direly need advanced and innovative solutions to combat fraud. Integrating NLP in insurance policy administration systems precisely solves the problem. This combination creates a powerful tool that effectively addresses the shortcomings of traditional insurance fraud detection systems. So, let's explore in detail how NLP-augmented policy administration solutions empower insurers to fight fraud.
Role of NLP in Combatting Fraud
Natural language processing lets algorithms understand and interpret natural language as humans do. Thus, it's no wonder that the NLP market size is expected to exceed $200 billion by 2031, growing at a CAGR of 25%. Now imagine adding these capabilities to traditional policy administration systems! These transform fraud detection through advanced linguistic analysis capabilities. Here's what all NLP can help with:
Enhanced Data Extraction and Analysis
Unlike traditional methods, an NLP-powered policy administration system in insurance can extract information from previously inaccessible unstructured data such as claim descriptions, medical reports, adjuster comments, etc. These systems identify inconsistencies between claim narratives and other documentation, revealing fraudsters' attempts at misrepresentation.
For instance, NLP tools can detect when injury details in claim forms contradict accompanying medical reports. These minute but significant contradictions often indicate fraud that might otherwise go unnoticed.
Sentiment and Linguistic Pattern Recognition
Sentiment analysis helps detect emotional clues that might point to fraud. For instance, signs like unusual language patterns, excessive details, overuse of qualifying statements, and passive voice trigger automatic alerts for further investigation. Additionally, emotional distancing language and unnecessary explanations in claim documentation also suggest fraudulent intent. Sentiment analysis is the best way to distinguish legitimate submissions from false ones.
NLP-based policy administration software can identify specific words and phrases often linked to fake claims. These language markers generally appear in multiple fraud attempts in similar situations. The advanced systems analyze semantic patterns that correlate with proven fraud cases. This builds an ever-growing knowledge base of linguistic signs associated with deceptive practices.
Entity and Relationship Mapping
There are instances when insurance fraud is coordinated and organized by multiple entities. Individual claim analysis might not be able to identify such a relationship network across seemingly unrelated claims. Thanks to the advanced capabilities of NLP-based systems, insurers can easily identify and verify relationships among claimants, witnesses, medical providers, and repair facilities.
Additionally, NLP systems excel at the temporal analysis of claim stories. They can detect when the order of events doesn't make sense or when timelines seem unlikely in descriptions of claimed incidents. These timing anomalies often reveal fake scenarios created to support false claims. The system identifies when described sequences have impossible logic or timing contradictions that human reviewers might miss.
Multilingual Processing and Risk Classification
In the context of international scams that usually breed from language barriers, NLP-enhanced insurance policy administration software stands out as an armored knight. It can effectively process multilingual communications with consistent accuracy, ensuring that detection capabilities remain effective, regardless of the document language. Additionally, claims receive risk scores based on comprehensive linguistic analysis. Thus, insurers can prioritize the most doubtful submissions and better focus investigative resources on high-risk cases.
Continuous Learning and Adaptation
What differentiates NLP-powered insurance policy administration solutions from traditional rule-based methods is their ability to learn and evolve. They have cross-referencing capabilities for automatic comparison between current claims and historical data. The system identifies patterns across seemingly unrelated claims that share suspicious characteristics. This comparative analysis reveals subtle similarities that might indicate coordinated fraud attempts or repeated tactics from known offenders.
The systems continuously learn from adjuster decisions and outcomes and improve through exposure to adjudicated cases. This creates increasingly accurate fraud detection models without requiring manual rule updates, thus ensuring detection capabilities remain current against evolving fraud techniques.
Final Thoughts
As insurance fraud rises, adding NLP to insurance policy administration software is not a fancy move but a smarter way to combat scams. In addition to identifying fraud, these advanced systems help boost efficiency and improve customer experiences while preventing financial losses and reputational damage. Even though shifting from traditional systems to new ones is challenging, the ROI quickly materializes through significant drops in fraud.