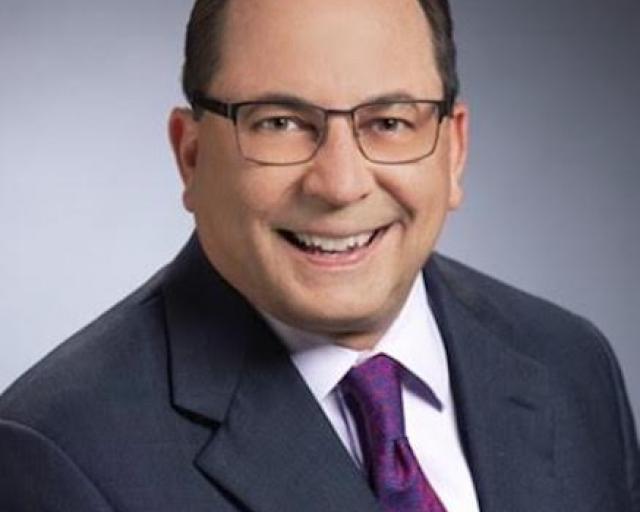
Tom Warden, the chief insurance and science officer at CLARA Analytics, is a big fan of artificial intelligence. But....
Therein lies a tale.
As Tom explains in the interview I did with him for this month's ITL Focus, AI is only as good as the data it works on, and most of the data being used for AI in insurance just isn't very good. The data for underwriting and claims comes largely from adjusters, who are evaluated and compensated primarily based on how quickly they resolve cases and may have more than 150 of them open at a time—not an environment conducive to producing highly accurate data or to making sure all the data fields required by an AI are filled in. Besides, AI needs three or four or five years of data to train itself on, and few insurers were addressing the data problem that long ago.
They aren't really addressing the problem now, either, because there are simply too many other pressing issues drawing the focus of adjusters and IT departments. So, while AI can be incredibly powerful, Tom says a lot of hard work has to be done before the industry sees the full benefits.
ITL:
A lot of talk about AI seems to treat it as fairy dust that you can sprinkle on things to get magic results, but you deal with this stuff day in and day out, so you see where the real benefits are—and where they aren't, at least just yet. What are the biggest benefits of AI thus far for insurance?
Tom Warden:
They’re still mostly in the underwriting space but claims is catching up fast. Companies are figuring out the fairy dust stuff isn't real, but they can make real progress if they carefully structure AI-based projects and implementations. They get the data right. They figure out the business problem that needs to be solved and make sure it's a real one, not some pie in the sky. They get all the necessary constituents in the room at the beginning—the data folks, the IT folks, obviously the data scientists, and people from the function that's going to be affected.
For the most part, you also need to keep the C-suite folks out of the room. You need their support, obviously, but don’t let them drive the train. They're the ones that are getting the most bombarded by the hype and all the marketing messages from vendors, so they can be unrealistic or impractical.
I mean, I once worked for a CEO who was very engaged and advocated for what I was doing, but his expectations about how fast we could go and how grand AI could be were inflated. He used to stop me and ask, "Tom, when are we going to be able to get rid of all the underwriters?" Or, "When can we get rid of all the adjusters?" He was partly kidding, but he really did talk a lot about increasing the productivity of adjusters and underwriters by factors of two or more. And that's just not feasible, at least in the near term. You can make great progress, but you must sort of nibble at it. I advocate for multiple problems being solved simultaneously, a portfolio approach, but each initiative needs its own resources.
His expectations were way out in front of what our capabilities were, especially because our database was a mess and our IT folks were having to do all sorts of other things—automate processes, build a new claims system, build a new underwriting system and so on.
You need to start, not by going top-down, but by going to the underwriters or the adjusters and asking how you can make their jobs easier and more productive. Thankfully, more and more companies are starting to figure that out.
ITL:
I want to follow up on your point about the messiness of data, because I think that's a key impediment to what AI can do. How do we solve that problem?
Warden:
I think it's the biggest issue, really.
Most of the claims data we ingest isn't from automated entry or from scanning documents. It's from adjusters. And these are people who all have 150 claims or more open at one time and who are pretty much compensated and evaluated based on how quickly they work. They're in a hurry. So, they don't always enter data accurately, or they don't fill in all the fields.
When you ask for three or four years of claims data so you can train the AI, you find you're dealing with all kinds of messy issues. Unfortunately, nobody with decision authority thought about the kind of data you’d need in the future for AI, or provided incentives to make sure that data was entered accurately. Cost minimization by IT departments is a big hindrance to collecting, cleaning and saving historic data.
ITL:
Are companies recognizing the problem and starting to make sure they produce the kind of clean data that AI needs?
Warden:
Not really, and it may be a while before they do. I had a fellow from a big insurer in the other day, and he just laughed when I asked if they were putting more rules in the claim system so adjusters couldn't skip over stuff or were forcing them to do data checks. He said that was a great idea, but it would take two years to update the legacy claim system, and there would be significant adjustments to workflows and incentives needed on top of that.
If a company is moving to a modern cloud system from Guidewire, Duck Creek or others, they have the opportunity to start fresh with new processes, and these systems can be changed more quickly. But even that is tricky. I know a chief claims officer who spent two and a half years implementing one of these systems, and he told me at the end, "Yeah, we had to leave a lot of stuff by the side of the road just to get it done." Some of that "stuff" was the checks on data accuracy and completeness.
I understand. You have to pay the claims and operate efficiently. But until people invest in data quality, they won't get the full value from the AI.
ITL:
Outside of what we've already discussed, where are you seeing real progress?
Warden:
The biggest improvements are probably on the customer service side, where you don't really need historical data to make the interaction with insurance companies easier. You can build chatbots or set up smarter paths through the call tree. Companies are also innovating in claims by having more and more decisions made automatically or by coaching adjusters without intervening.
ITL:
I was a big M*A*S*H fan growing up, which is probably where I learned the term "triage." I think of the term as relevant to AI in insurance. You divide problems into three sorts—ones that can be resolved immediately by AI, ones that should immediately be sent to a human expert and ones in the middle that can maybe involve some combination of people and AI. Initially, there may not be very many in the AI-only bucket, but you hope that, over time, you'll keep learning and keep moving more into that realm. Does that notion match what you're seeing?
Warden:
Yes, and you don't always even need a true AI-based solution. You can build an expert system by just interviewing adjusters and figuring how what rules to apply in certain circumstances and get 80% of the lift that you'd get from a more elaborate, AI system. Then, with enough time, we can add the AI on top of it to find the subtle things that are predictive and useful that maybe no one's thought of.
But people have it backward. They think, oh, AI is the answer. No, if you just mechanize your decision rules and have everyone follow them, that's where most of the lift is. AI can take you to higher levels, but it needs a decision-focused base to build from.
ITL:
Thanks, Tom.