While current market opportunities for insurers – and for insurtechs – require a good product to sell, a large part of the story is about accessing customers via their preferred channels. So the topic of distribution is a natural follow
-up to our last post on
marketing and customer-centricity.
The pre
-digital era was characterized by more of a captive, sellers’ market, in which customers had little choice but to seek insurance via their agent of choice, who in turn would funnel work to a small number of large incumbents, generally ignoring new entrants.
Over the past years, though, we have seen either the outright emergence or the rapid expansion of a number of non-traditional channels, encompassing direct
-to
-customer channels offered by insurers, new insurtech propositions, aggregator sites and affinity partnerships with major brands and retailers.
So how exactly has this sea change in distribution changed the game for incumbents?
Since the start of the internet, the insurance industry has invested in and expanded its digital channels from company websites to comparison sites, aggregators, social media and more – all in an effort to capture new business. At the same time, insurance remains a complex product that is hard to research, buy and use. This is an enormous problem for the insurance industry because every gap and point of complexity is a giant bull’s
-eye for alternative channels, insurtechs and new managing general agencies (MGAs).
"Those who can make insurance easier for customers to understand and buy stand a good chance of capturing business from companies whose processes remain complex. In today’s new digital world, it is not about any single channel but rather about a multichannel approach that is based on consumer choice." – Denise Garth, SVP of strategic marketing, industry relations and innovation at Majesco
The emergence of new channels has raised the stakes for incumbent insurers, nimble newcomers and players outside of insurance alike, all of whom have an opportunity to capitalize or, otherwise, get left behind. In this installment, on distribution, we examine:
- The rise of the digital direct channel
- The expanding role of affiliate partnerships
- The importance of cross-channel consistency for insurers
- Carriers' omnichannel strategies
- The impact of aggregators
- How distribution is driving disruption
Our stats and outside perspectives are drawn from our Global Trend Map; a breakdown of all survey respondents, and details of our methodology, are included in the full Trend Map, which you can download for free at any time.
1. Going Direct to Customer
72% of insurers sell to customers directly…
We can see that the direct channel has become a totally mainstream concern for insurers. Interestingly – and based on our segmented stats – North America appears to trail on this measure compared with our other regions, in conformity with our prediction from the our last installment, on
marketing and customer-centricity: namely that channel disruption is potentially less in North America.
The strong showing for direct channels in Asia
-Pacific is interesting as, from our broader research with contacts in the region, we know the market there to be heavily intermediated, with a strong reliance on agencies and, in particular, bancassurance. For example, recent research from Swiss Re and LIMRA indicated that the direct channel does not exceed 10% of total share in any APAC national market apart from China.
We should bear in mind that our stat indicates the
existence of the direct channel rather than its volume. Nevertheless, for a healthy number of APAC insurers to have established a direct channel, despite what remain for now relatively low volumes of business, indicates how strategic this channel is perceived to be. We may remember, as well, from our priority tables, that Asia
-Pacific led our other regions on distribution diversification, which adds weight to this trend (see
Global Trend Map No. 3: Priorities).
"The reach of this digital transformation goes way beyond the elimination of 'the middle man' from a distribution point of view. The direct digital channel dominates very few markets and deals only with compulsory insurance. In the vast majority of markets, a multichannel-oriented customer continues — with variations from country to country — to choose at least at some point of the customer journey to interact with an intermediary." – Matteo Carbone, founder and director at Connected Insurance Observatory
While many customers in many circumstances may prefer the direct channel to the agency path, insurers should not necessarily place all their strategic eggs in this one basket. Insurance has always been sold, as they say, and never bought, so any portal for buying insurance, however slick, is at a disadvantage by its very nature.
See also: Distribution: About To Get Personal
The way to get insurance products into customers’ hands may, in fact, be to integrate them into other products that
are bought, whereby the insurance becomes part of a bundle or an add-on.
This philosophy has boosted the popularity of affiliate channels, which, in addition to taking even more friction out of the process, also bypass any issues that may exist with consumer trust, by tying the insurance to a trusted brand that consumers know, respect and perhaps already interact with daily or weekly.
2. Expanding Affiliate Channels
89% of insurer respondents are increasing their distribution through affiliate partners …
Current examples of affiliate channels are major retailers, such as Tesco in the U.K. and Falabella in South America, but theoretically the affiliate channel could include just about anything, with the insurer effectively becoming an API that other consumer applications can plug into, like for instance ride
-sharing and taxi apps for travel insurance.
The scale that incumbent insurers can offer in this channel may put them in good stead against their insurtech competitors; large affiliates can benefit from the brand equity of household
-name insurers, and the resultant selling partnership will likely prove more successful for all involved.
"We're looking into partnerships with companies from different sectors: how we can plug in, bringing the insurance dimension and being the insurance carrier, while the partner does all the front-end, customer-facing stuff. And as I like to call it, we're just a third-party API." – João Neiva, head of innovation, IT and business change at Zurich Topas Life
Another important indirect channel – but one on which we have not gathered stats – is bancassurance. While the concept is making headway in emerging markets, it has been out of fashion in Western markets over the past decade. The interest expressed this January by Italian bank Intesa Sanpaolo in a tie
-up with Assicurazioni Generali shows the concept is not dead – but this deal was nonetheless scrapped the following month.
3. The Omni-Channel Grail: Consistent Multi-Channel Experiences
As of today, many insurers operate both direct
-to
-customer and affiliate channels alongside their traditional agency channels. Whatever the blend of channels that customers ultimately come through, it is important for insurers to offer a consistent experience across all of them (a consistent experience need not necessarily be an identical one).
It’s bad enough if one channel offers a comparatively poor or irregular service, this is then compounded because consumers are increasingly – as in retail and e
-commerce – using multiple channels as part of their research and decision-making process, and an inconsistent (or in any way confusing) experience will lead valuable customers to bounce or churn.
In certain segments, a majority of customers may well come through a broker/agency channel for the foreseeable future, but it would be unwise to ignore the role of the direct channel in prepping them and to neglect obvious re
-engagement points during the process that can recall, reinforce and build on the online experience.
"We believe that this is an opportunity for brokers and intermediaries to innovate and continue to create new sources of value for their B2C and B2B segments. For instance, identifying and carving out new and emerging B2C (micro-insurance, flood, non-standard risks, risk pools/schemes, older generation/retirees) and B2B (IP-based startups, cyber, supply chain, cross-border liability, terrorism) needs and creating innovative channels to access them." – Sam Evans, managing director at Eos Venture Partners
While much of insurers’ backroom tech can be aligned across channels, the face
-to
-face element in indirect channels can prove more challenging to coordinate, especially as we are here dealing with a multitude of different selling organizations with a multitude of different working cultures.
This is not to say that the face
-to
-face element is a tale of lost opportunities and inefficiencies – if it’s put to work effectively, there’s seldom a better way to create lasting customer engagement and up-selling opportunities.
So, Is Your Customer Experience Consistent Across Channels?
Customer experience (CX) professionals in insurance are chasing the same omni-channel grail as their analogues in other digitally disrupted industries, like retail/e
-commerce, that is: to ensure that customers enjoy the same product and service experience regardless of which channel they come through. Let’s start by seeing how well Insurers currently perform in this regard:
Only 23% of insurers believe their customer experience is consistent across channels …

There is clearly still a long way to go before omni-channel is the norm in insurance, and the steady addition of new channels will further complicate matters for insurers chasing channel consistency.
"Insurers’ infrastructure, which has been built over literally hundreds of years, never anticipated having multiple channels of communication to support, so insurers are scrambling to learn how to do that." – Stephen Applebaum, managing partner at Insurance Solutions Group
From our regional segmentation, we can reveal that Asia
-Pacific trails our other regions on this measure. This is likely a consequence of the pursuit of new channels in the region (as we noted with the prevalence of the direct
-to
-customer channel): It is more difficult to maintain consistency across a multitude of emerging channels than across a core of traditional ones.
4. Do You Have an Omni-Channel Strategy?
The creation of an explicit omni-channel strategy is the first step of many toward being able to offer a consistent customer experience (CX) across channels.
62% of insurers have an omni-channel strategy…
It is encouraging to see that the majority of insurers do have formal omni-channel strategies, and this should go a long way toward raising the low percentage of insurers currently able to offer a consistent customer experience across channels.

It will likely be a number of years before today's omni-channel strategies yield concrete results, and, as we pointed out, the continuing complication of the distribution landscape through the addition of new channels will mean insurers must run just to stay where they are.
"Most insurers are still focused on e-commerce, but the leaders are developing longer-lasting relationships by using their digital capabilities to gain enhanced customer knowledge and harnessing that information to profile customers more effectively, fine-tune underwriting and deliver customized solutions." – Michael Quindazzi, business development leader and management consultant at PwC
5. Attack of the Aggregators!
Our final question on distribution relates to the role of aggregators like U.K.
-based comparethemarket.com, U.S.
-based comparenow.com and Singapore
-based GoBear. These have burgeoned since the millennium, inserting an extra distributional step between insurers and their prospective clients, and have had a major impact on the market (just like comparison sites in other industries) both in terms of the overall business model and from a branding and customer
-relationship perspective. By allowing, and encouraging, customers to pit insurers against each other on a price
-by
-price basis, these sites have further commoditized insurance lines and driven down premium prices and margins.
"The process of buying insurance can be simple – go online, compare the relevant information, select an insurer and pay. But three days later you get a 22-page printed policy at home, written by a lawyer. As a layman, you’re totally lost. What customers really want are simpler and easy-to-understand products so that they regain trust in this industry. Get that trust, and it will drive revenues." – Andre Hesselink, CEO at GoBear
Due to a variety of factors, including marketing budgets and regulation, the effects of aggregators are neither uniform across lines nor across geographies. For example, according to a recent survey of consumers by consultancy Finaccord, more than 40% of respondents in the U.K. had taken out car insurance via an aggregator, compared with only 5% in the U.S. and Canada.

The impact of aggregators can be felt across the whole ecosystem, so we asked all our respondents to specify how big an impact they are having on their organizations. Overall, 14% indicated a large impact, 29% a medium one, 37% a small one and 20% none at all. As we can see from the infographic above, a relatively small proportion of the ecosystem is heavily affected, although the impact is being widely felt (more than three quarters of respondents citing some impact).
See also: Taking the ‘I’ Out of Insurance Distribution
From our regional segmentation, we can reveal that Asia
-Pacific trails on this measure. As we have pointed out, while many insurers there do have digital channels, the overall volume of business being done this way is still quite low – and this potentially explains the lower regional score. However, as insurers in the region actively build and promote their direct capabilities, we expect aggregator impact there to quickly catch up.
6. Distribution: The Fulcrum of Market Disruption?
We suggested in our previous post on
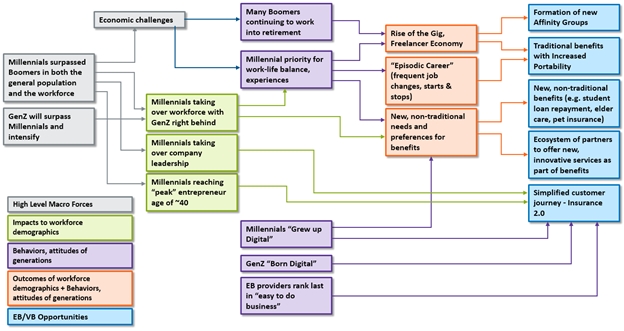
marketing and customer-centricity that changes to distribution are what fundamentally lies behind today's changing customer expectations and behaviors (specifically the internet and the rise of digital for everything from research to commerce).
"The most important driver of success for insurtech start-ups has been distribution. Distribution in insurance (more specifically in personal lines, but increasingly so in commercial lines) is getting disintermediated as data becomes increasingly transparent between the buyer and seller." – Sam Evans, managing director at Eos Venture Partners
As a result, we predicted that traditional channels might be marginally more intact in North America than elsewhere – as an explanation for this region's marginally lesser prioritization of the customer (as we saw from our priority tables in
Global Trend Map No. 3: Priorities). Our reasoning: If new channels are the fundamental enablers of disruption, the more stable the traditional channels are, the less disruption insurers will face and therefore the less forcefully they will have to prioritize the customer.
So, what do our regional stats on distribution reveal? ...
We noted that the direct
-to
-customer channel is less prevalent in North America than elsewhere, so it would indeed appear that traditional distribution is – marginally – more intact here.
This strength of traditional channels translates into lower levels of lost business for North American carriers. Indeed, in our earlier post on insurtech –
Global Trend Map No. 2: Insurtech – where we introduced the "disruption score," only a quarter of insurers and reinsurers in North America reported losing market share to new entrants (versus 47% in Asia
-Pacific).
The model we are applying is one in which distribution disruption leads to customer disruption and thereby to a complete re
-evaluation of the customer relationship. So, what can this tell us about Europe and Asia-Pacific?
Let us start with Asia
-Pacific: On the distribution level, we encounter a high incidence of direct channels, low channel consistency and a high priority allocated to distribution diversification (as we saw from our priority tables in
Global Trend Map No. 3: Priorities). And following this through, we find a corresponding degree of disruption on the customer level, with APAC respondents scoring high on measures of customer priority (as we saw in the previous section on
marketing and customer-centricity).
It is clear, therefore, that APAC insurers know they are in trouble and that they are trying to meet the 21st-century consumer head-on. This is very much in line with our disruption score for the region, whereby 47% of in Asia-Pacific stated that they were losing market share to new entrants, a high score in which fear may well play a considerable role.
Europe is an interesting case. In terms of distribution, we note solid adoption of direct
-to
-customer channels, and the continent has in many ways been a pioneer in its use of affiliate channels and aggregators (we explore these themes in more depth in our regional profile
on Europe – read ahead
here). The customer relationship here (along with Asia-Pacific) is marginally more problematic than in North America, based on the forceful prioritization of the customer we found here.
Does this mean that Europe finds itself in the relatively more disrupted camp, along with Asia-Pacific? Not necessarily.
We cannot help but notice Europe’s low disruption score of 23% (much lower than Asia-Pacific's, in line with North America), meaning that, at least in carriers' perceptions, relatively little market share is currently being lost. One way to square this with our foregoing observations on the distribution and customer situation in Europe would be if European insurers were rising better to the challenge of serving customers across a complex distribution landscape than their counterparts in Asia
-Pacific are.
This would imply that Europe is perhaps slightly ahead of the curve and has had some time to adjust. In line with this hypothesis is the low prominence of the chief customer officer role among recent or forthcoming appointments at European insurers (contrasting with its importance in Asia
-Pacific). Our inference from this is not that customer
-related roles do not exist in Europe (after all, Europe allocated the highest overall priority to customer-centricity out of all our regions) but rather that they are not of such recent creation.
So, we can tentatively conclude that, while Europe and Asia
-Pacific are both undergoing distribution
- and customer
-driven disruption, Europe has entered deeper into this. There is, as such, no wholesale panic regarding lost market share through new entrants. In this sense, Europe would be not so much the most disrupted as the longest-disrupted of our key regions.
It will be interesting to observe how the sense of disruption in Europe, North America and Asia
-Pacific waxes and wanes as the market develops. The characterization we have attempted here is based on fine gradations, and, with the global market fluctuating as it is, there is no reason to believe development in any region will be linear. We return to these issues – and to the perennial question of disruption – in the regional profiles section with which we close the report (read ahead
here).
"Technology is changing more rapidly today than ever, which is changing the nature of risk. The distribution of insurance products and services is poised for rapid change. Agents and brokers will have a role to play as the distribution model changes. Those agents and brokers that are willing to adapt will thrive, those that rely on the old methods will continue to be successful until they wake up one day and they are not." – Steve Anderson, president at the Anderson Network
As insurers around the world pursue customers, we are left with the question of the brokers and agents who hitherto have been the face of the insurance industry.
Intermediaries still hold the cards in many customer segments and business lines – especially for complex, high
-value products in life and commercial – and can play an important role more broadly as part of the omni-channel mix. And, before we write them off too hastily, we should remember one thing: Although intermediaries no longer own distribution in the strictest sense, it is debatable whether carriers will want to take all aspects of customer-servicing in house just because they can.
"Chatbots and guided conversations – in the not-too-distant future – will significantly change the role of agents and brokers when providing insurance knowledge and resources to policyholders. Expert advice will still be needed, but chatbots and guided conversations will provide much of the basic information to the digital-savvy consumer anytime and anywhere." – Steve Anderson
For insurance players big and small, distribution is the key to getting in front of today's customers, in the sense either of tapping totally new segments or of fighting off competitors' threats to the existing book. However, if you cannot follow up on your promises across the customer life
-cycle, then all that top
-of
-funnel work will have been in vain.