Following on from our previous post on
product development, which concluded the key themes section of our Global Trend Map, we now examine the insurance and insurtech trends in the world's major markets via our dedicated regional profiles. We focus on seven key regions.

In our forthcoming posts, we will be referring back — on a regional and comparative basis — to the stats presented across our earlier installments on: Industry Challenges, Insurtech Perspectives, Insurer Priorities, Services, Investments & Job Roles, Analytics & AI, Digital Innovation, Internet of Things, Marketing & Customer-Centricity, Distribution, Claims, Fraud, Cybersecurity, Investment Management, Regulation and Product Development. Additionally, we supplement our statistics with perspectives and discussion from a range of local correspondents in each region.
In this post, which introduces our regional profiles, we present a brief preview of each region including key external and internal challenges, as well as insurer priorities. Each preview kicks off with a Top-Trumps-style summary table of key stats (an exhaustive key explaining each measure is included in the
full report).

In our
Profile on Europe, we draw on the expert opinions of Switzerland-based venture capitalist Spiros Margaris, VC (InsureScan.net, moneymeets & kapilendo), and Charlotte Halkett, former General Manager of Communications at UK-based telematics provider Insure The Box (now MD of Buzzvault at Buzzmove). For all their insights, simply download the full version of the report. Below is a sneak preview of the stats and themes we discuss in the full profile.
"Europe presents us with a potentially gloomy picture, with the on-going issues of low interest rates and weak growth prospects, to which we may add growing regulatory burdens and political uncertainty – especially in the wake of the UK’s Brexit vote. However, we have nonetheless gathered plenty of evidence that incumbents have the tools in place both to come through and to hold their own against new entrants." — Helen Raff, Head of Content at Insurance Nexus
i) The External Challenges: Europe
In Europe, the top three external challenges facing the insurance industry as a whole follow the global trend we outlined in our
earlier post on Industry Challenges: 'Technological advancement', 'Changing customer expectations' and 'Digital channel capabilities'.
Looking further down the table, some points of note are the higher position attained by ‘Increased regulation’ and the lower positions of ‘New emerging risks’ and ‘Catastrophe risk’. Compared to some of the other regions we examine, like Africa and Asia-Pacific, Europe is relatively sheltered from natural catastrophes and the associated risks that they bring with them, which possibly explains the lower scores we find for ‘New emerging risks’ and ‘Catastrophe risk’.
As for the prominence of the regulatory challenge, we need look no further than the EU’s Solvency II, which came into effect at the start of 2016 and represents the first major shakeup of the landscape since the 1970s.
--- ii) The Internal Challenges: Europe
Internally, the top challenges are close to the global trend we outlined in our
earlier post on Industry Challenges: ‘Lack of innovation capabilities’ and ‘Legacy systems’ take first and second place respectively, with ‘Siloed operations’ edging out ‘Finding and hiring talent’in third place.
 --- iii) Insurer Priorities: Europe
--- iii) Insurer Priorities: Europe
These are the priority areas on which European insurers lead our other regions, out of our shortlist of 15 priority areas presented in our
earlier post on Insurer Priorities:
"Customer-centricity is an important issue because insurance is a 'trusted good'. To address social values and preferences is important. Customer-centricity means building trust, branding and a business model based on relational values. Not for nothing: Empirical evidence shows that identity is the strongest customer KPI." — Andreas Staub, Manager Partner at FehrAdvice
In our
full profile for Europe, we dig deeper into these challenges and priority areas on a more qualitative note, with insights from our two regional contributors, Spiros Margarisand Charlotte Halkett. Key focal points of our discussion include:
- Growth opportunities in a relatively saturated market
- The European consumer and Europe’s ‘early adopter’ status
- How European insurers are using new technologies to deliver on their customer promise
- Dynamic, real-time insurance and IoT
- Progress on developing connected insurance models across the continent as a whole
NORTH AMERICA PROFILE: Preview
In our profile on North America, we corroborate, and expand on, our stats via the seasoned perspectives of Chicago-based Stephen Applebaum, Managing Partner at Insurance Solutions Group, and Boston-based Matthew Josefowicz, CEO at Novarica. Below is a sneak preview of the themes we tackle in the full profile.
"Rising claims costs – both attritional and catastrophic – against a backdrop of low interest rates calls for a new approach to insurance in North America. That the lion’s share of Insurtech deal money has been going to US companies suggests that this change of approach may not be long in coming." — Marsha Irving, Head of Innovation / Commercial Director at Insurance Nexus
--- i) The External Challenges: North America

In North America, the top external challenges for the insurance sector as a whole follow the global trend from our
earlier post on Industry Challenges, with ‘Technological advancement’ and ‘Changing customer expectations’ taking 1st and 2nd place respectively, except that in 3rd place we find ‘New emerging risks’. In comparison, this comes 4th globally and only makes 6th place in Europe – which, as we indicated in our Europe preview above, likely reflects some parts of the world being more exposed to disasters (and hence concomitant risks) than others. Further down the table, 'Increased competition' moves up a place, knocking 'Increased regulation' down one spot to 7th.
See also: How Is Insurtech Different in Asia?
--- ii) The Internal Challenges: North America
Looking internally, the top challenges reflect the global trend we outlined in our
earlier post on Industry Challenges, except that ‘Legacy systems’ wrests the top slot from ‘Lack of innovation capabilities’ (which, by way of comparison, comes first in Europe and Asia-Pacific).

Innovation is, at its heart, customer-driven, and, as part of our Regional Profiles, we compare the insurer-customer relationship in North America with what we find in our other key regions – and this may well explain the different positions ascribed to ‘Lack of innovation capabilities’ in their respective challenge tables. The parallel suggestion is that ‘Legacy systems’ play more of a role in North America, which is another theme our full profile investigates in more depth.
"Legacy systems has long been a core challenge for executives across functions within insurance carriers who are focused on innovation, customer experience and efficiency. Impacting product development, applying analytics, claims modernization, marketing optimization and more, it’s no surprise this is such a top priority for insurers. In the future, I think we’ll see more legacy system upgrades across insurers looking to digitize and streamline operations." —Emma Sheard, Head of Strategy at Insurance Nexus
--- iii) Insurer Priorities: North America
These are the priority areas on which North American insurers lead our other regions, out of our shortlist of 15 priority areas as presented in our
earlier post on Insurer Priorities:

In our full profile for North America, we return to these challenges and priority areas, bouncing them off our two regional contributors, Stephen Applebaum and Matthew Josefowicz. Some of our key points of interest that emerge, and which we discuss in detail, are:
- Insurers’ renewed focus on their primary underwriting business in the face of low interest rates and impending market disruption
- The rise of the ‘new consumer’ and how this is changing the insurer-customer relationship
- Customer-centricity as the prime mover of distribution and product
- The impact of legacy systems and regulation on (re)insurers’ innovation and transformation efforts
- How insurers are to unlock new sources of growth in a mature market
ASIA-PACIFIC PROFILE: Preview

Our exploration of Asia-Pacific brings into play, alongside our statistics, the experience and perspectives of three in-region commentators: Steve Tunstall, CEO at Singapore-based Insurtech start-up Inzsure, João Neiva, Head of Innovation, IT and Business Change at Zurich Topas Life in Indonesia, and HK-based David Piesse, Chairman of IIS Ambassadors &Ambassador Asia Pacific at the International Insurance Society (IIS). What follows is a preview of our Asia-Pacific Profile (full thing
here).
--- i) The External Challenges: Asia-Pacific
In Asia-Pacific, the top external challenges facing insurance as a whole follow the global trend familiar from our
earlier post on Industry Challenges, with ‘Technological advancement’ and ‘Changing customer expectations’ taking first and second place respectively, except that, as in North America, in third place we find ‘New emerging risks’(by way of comparison, this challenge only makes 6th place in Europe).

One possible explanation for the higher ranking of ‘New emerging risks’ is to be found in the related challenge of ‘Catastrophe risk’ – which also results one place higher in Asia-Pacific than was the global trend.
While natural catastrophes are not emerging risks, in the sense that they have always occurred, their consequences are becoming more multifaceted as a result of the massive growth in urban areas and the rife interconnection of business in today’s globalised economy. This has introduced a new class of accumulation risk which could justifiably be called ‘emerging’.
We know anecdotally that this phenomenon is particularly pronounced in the APAC region, which boasts some of the densest urban and business conglomerations in the world, in and among noted catastrophe zones, and the trend towards urbanisation and megacities is only set to continue.
See also: Insurtech Ecosystem Emerging in Asia
Another detail we notice with the external challenges is the relatively high position attained by ‘Increased competition’ (two places up on the global trend), and we believe this is a natural consequence of the expansion opportunities on offer in the region. As we uncover in the course of our full Regional Profile for Asia-Pacific, this uneasy marriage of high growth and high competition is in many ways APAC’s defining market characteristic: to win is only ever to win big (
get the full profile).
"The most significant challenges for insurers in Asia, from an IT perspective are: firstly, moving services to online sales – for agents, brokers, bancassurance and direct to customers; secondly, providing instant and ideally paperless servicing on claims management; and finally, the development of Chinese Insurtech players if they decide to compete outside of their local market." — Ash Shah, Regional CIO and Chief of Staff Property and Casualty at AXA Asia
--- ii) The Internal Challenges: Asia-Pacific
The internal challenges highlighted by APAC respondents exactly replicate the global trend we staked out in earlier post on Industry Challenges, with a top three constituted by: ‘Lack of innovation capabilities’, ‘Legacy systems’ and ‘Finding and hiring talent’.
 --- iii) Insurer Priorities: Asia-Pacific
--- iii) Insurer Priorities: Asia-Pacific
The following 6 priority areas are those on which insurers in Asia-Pacific lead our other regions, out of our shortlist of 15 priority areas introduced in our earlier post on Insurer Priorities:
 "Doing nothing is not an option any longer. The top priority for many CEOs is to acquire the capabilities to deliver true digital innovation that achieves competitive advantage in a very short period of time. Understanding the agile and flexible lean techniques used within the start-up world can help. Analytics, the IoT or mobile are just enablers to ease such transformation." — Sabine VanderLinden, Managing Director at Startupbootcamp
"Doing nothing is not an option any longer. The top priority for many CEOs is to acquire the capabilities to deliver true digital innovation that achieves competitive advantage in a very short period of time. Understanding the agile and flexible lean techniques used within the start-up world can help. Analytics, the IoT or mobile are just enablers to ease such transformation." — Sabine VanderLinden, Managing Director at Startupbootcamp
We return to these regional constellation of challenges and priority areas in our full Regional Profile for Asia-Pac, in which we present the direct market testimonies of Steve Tunstall, Joao Neiva and David Piesse. Key areas that we drill down into are:
- The high-growth, high-competition dynamic inherent in the Asia-Pacific insurance market
- The new calling for customer-centricity and the related question of disruption
- Using data and analytics to create more customer-centric products, such as personalised, on-demand insurance
- APAC distribution landscape and what insurers are doing to ensure scale for their products
- How to successfully manage back-office digital transformation
PROFILES FOR LATAM, MIDDLE EAST, AFRICA AND CENTRAL ASIA
We are unable, given the constraints of this post, to provide full previews of our profiles for these regions. Suffice it to say, like the profiles that are presented here, they are fundamentally structured around discussion with in-region correspondents:
--- LATAM
Luiz Bruzadin, Founder at Brazil-based Insurtech Segure.me, and Hilario Itriago, CEO at VC fund Bullfrog Venture
--- MIDDLE EAST
Cherian John, 2017-18 Regional Chairman - Europe, Middle East & Africa at Million Dollar Round Table (MDRT), Ahmad Al-Qarishi, Chief Risk Officer and Chief Actuary at Saudi Re, and Israel-based Dani Cozer, Reinsurance Operations at I.D.I. Direct Insurance
--- AFRICA
George Otieno Ochieng, Claims Manager at Britam General Insurance Company, and Belhassen Tonat, Head of Non-Life at Munich Reinsurance Company of Africa Ltd
--- CENTRAL ASIA
Kevin Hartnett, Chief Operating Officer at The Insurance Corporation of Afghanistan (ICA)
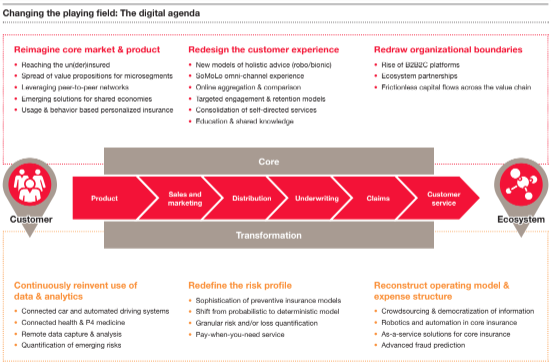
 Carriers’ initial response has been to drive profitable growth by streamlining their operating models and making incremental investments in technology to upgrade their capabilities. However, employer and employee needs and expectations continue to rise.
Employers are using innovative benefit solutions to differentiate themselves when recruiting and retaining top talent. Employers recognize that employees no longer have the patience or time for benefit plans that are cumbersome to enroll in and manage. They’re looking for holistic solutions that employees themselves can direct. In addition, employees have different needs based on income diversity and – more so than in recent memory – generational circumstances. Consequently, they’re looking to employers to offer customizable solutions that help them meet their unique needs in a user-friendly fashion, 24/7.
Moving forward, five trends will continue to shape the group insurance market and influence carriers to move beyond incremental investment to fundamentally reposition their business and operating models. These trends will motivate group insurers to provide more measurable value for employers, employees and intermediaries by delivering more integrated products and services and better customer experiences. We also expect to see a) More and more players in adjacent markets such as health, workforce management and wealth to expand into market niches that overlap with group insurance; and b) More venture capital to flow to insurtech solutions that meet the group space’s evolving needs.
Group insurer solutions will take advantage of the convergence of
health-wealth-career management
Consumers are increasingly managing their health, wealth and career decisions in a coordinated way because they all affect the same wallet.
Decisions about health range from ways to maintain fitness to ensure their quality of life (and thus ability earn an income) to selecting the right combination of benefit products to reduce the key risks that could knock them and their families off track for an extended period of time. As people at the higher end of the socioeconomic scale live longer and healthier lives, they’re looking to manage their personal wealth to support their and their families’ financial positions for longer periods of time.
Moreover, as employers compete for top talent, they are increasingly providing benefits and programs that address the concerns their employees have about their and their families’ physical, mental and financial health. Employers are focusing on a) health and return to work programs that contribute to worker productivity and performance, and b) employee development programs.
See also: How to Unlock Group Insurance Market
The confluence of these factors is creating opportunities for group insurers to provide employers with solutions that help them improve their employees’ health, wealth and professional satisfaction. Some carriers are responding by offering more holistic solutions, either by expanding their own product offerings or through partnerships with others in which they can white label products. Other carriers have decided not to expand their own product offerings, but instead focus more on the wealth/ retirement or health. In either case, they’re trying to make their products and services fit with the other benefits employers’ chosen platforms offer.
Carriers’ initial response has been to drive profitable growth by streamlining their operating models and making incremental investments in technology to upgrade their capabilities. However, employer and employee needs and expectations continue to rise.
Employers are using innovative benefit solutions to differentiate themselves when recruiting and retaining top talent. Employers recognize that employees no longer have the patience or time for benefit plans that are cumbersome to enroll in and manage. They’re looking for holistic solutions that employees themselves can direct. In addition, employees have different needs based on income diversity and – more so than in recent memory – generational circumstances. Consequently, they’re looking to employers to offer customizable solutions that help them meet their unique needs in a user-friendly fashion, 24/7.
Moving forward, five trends will continue to shape the group insurance market and influence carriers to move beyond incremental investment to fundamentally reposition their business and operating models. These trends will motivate group insurers to provide more measurable value for employers, employees and intermediaries by delivering more integrated products and services and better customer experiences. We also expect to see a) More and more players in adjacent markets such as health, workforce management and wealth to expand into market niches that overlap with group insurance; and b) More venture capital to flow to insurtech solutions that meet the group space’s evolving needs.
Group insurer solutions will take advantage of the convergence of
health-wealth-career management
Consumers are increasingly managing their health, wealth and career decisions in a coordinated way because they all affect the same wallet.
Decisions about health range from ways to maintain fitness to ensure their quality of life (and thus ability earn an income) to selecting the right combination of benefit products to reduce the key risks that could knock them and their families off track for an extended period of time. As people at the higher end of the socioeconomic scale live longer and healthier lives, they’re looking to manage their personal wealth to support their and their families’ financial positions for longer periods of time.
Moreover, as employers compete for top talent, they are increasingly providing benefits and programs that address the concerns their employees have about their and their families’ physical, mental and financial health. Employers are focusing on a) health and return to work programs that contribute to worker productivity and performance, and b) employee development programs.
See also: How to Unlock Group Insurance Market
The confluence of these factors is creating opportunities for group insurers to provide employers with solutions that help them improve their employees’ health, wealth and professional satisfaction. Some carriers are responding by offering more holistic solutions, either by expanding their own product offerings or through partnerships with others in which they can white label products. Other carriers have decided not to expand their own product offerings, but instead focus more on the wealth/ retirement or health. In either case, they’re trying to make their products and services fit with the other benefits employers’ chosen platforms offer.
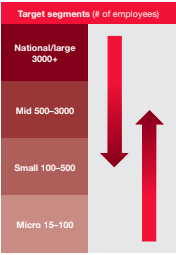
 Group insurers will look to serve more market segments
Many group insurers have long focused on certain market segments. For example, some have been dominant in the national account or large case segments and others in the small or mid-case account segments.
Each market segment requires different operating model strengths. But, as employer and employee needs increasingly change, the traditional lines between small, mid, and large account segments are starting to blur.
Group carriers are now rebuilding core capabilities and introducing new ones in order to more profitably serve a broader range of employer segments. Recent M&A activity has resulted in significant new capabilities. For example, the Hartford, which acquired Aetna’s group life and disability business, and Lincoln Financial Group, which acquired Liberty Life, are examples of the priority group players are placing on adding or enhancing capabilities (such as integrated absence management) to serve broader segments of the market.
These moves indicate that the carriers which traditionally have been stronger in the small and mid-markets are building new capabilities and transforming their target operating models in order to serve the unique needs of larger account segments. Moreover, large account carriers are building new capabilities and changing their target operating models in order to standardize and automate their solutions to more profitably serve smaller market segments.
Group insurers will look to serve more market segments
Many group insurers have long focused on certain market segments. For example, some have been dominant in the national account or large case segments and others in the small or mid-case account segments.
Each market segment requires different operating model strengths. But, as employer and employee needs increasingly change, the traditional lines between small, mid, and large account segments are starting to blur.
Group carriers are now rebuilding core capabilities and introducing new ones in order to more profitably serve a broader range of employer segments. Recent M&A activity has resulted in significant new capabilities. For example, the Hartford, which acquired Aetna’s group life and disability business, and Lincoln Financial Group, which acquired Liberty Life, are examples of the priority group players are placing on adding or enhancing capabilities (such as integrated absence management) to serve broader segments of the market.
These moves indicate that the carriers which traditionally have been stronger in the small and mid-markets are building new capabilities and transforming their target operating models in order to serve the unique needs of larger account segments. Moreover, large account carriers are building new capabilities and changing their target operating models in order to standardize and automate their solutions to more profitably serve smaller market segments.
 Group insurers will increasingly respond to increased absence management needs, even for down market clients
Absence and leave management services are a core service in the disability market and demand is growing.
There has been a spike in requests by employers for absence and leave services as a result of:
a. The January 1, 2018 New York Paid Family Leave Law, which is the most significant paid leave program in the US;
b. Recent localized laws, such as the Paid Sick Leave Ordinance (PSLO) and Paid Parental Leave Ordinance, have increased the local complexity of employer leave and absence tracking; and
c. Increased cross-selling of disability, FMLA, and voluntary products makes the need for claims/absence integrated services more relevant.
In response to these changes, carriers are increasingly adding absence services and platforms to their repertoire. For those familiar with disability, FMLA, and other products, absence is not new. For those who aren’t, tracking the high number of federal, state, and local laws is a tremendous value-add to their client base. In order to improve customer service, carriers are integrating claims and absence into an “event” experience to radically reduce the burden of correspondence that explains payments and absence rights.
M&A activity and insurtech investment will continue to shape in the group market
Moving upstream and downstream among employer segments requires new capabilities.
The traditional way of doing business will not meet changing employer and employee expectations. As a result, M&A, insurtech investment, and maturing group technology solutions will continue to influence the group market in three ways:
a. In addition to the M&A activity we previously noted, there have been other transactions in the group space, including Meiji’s acquisition of Stancorp and Sumitomo Life’s acquisition of Symetra. Acquisitions like these potentially provide much needed capital investment for group players looking to take advantage of the convergence in the space and the opportunity to profitably expand across traditional market segments. This in turn could raise the bar for existing players, especially in areas where they need i) broker or consultant customers to recommend their products, and ii) to address employer needs to respond the changing employer- employee dynamic.
b. There also have been deals adjacent to group benefits, such as CVS’s acquisition of Aetna and the Amazon, Berkshire and JP Morgan joint venture. These developments may impact more than product solutions, pricing and omni-channel distribution and service; they also could significantly reshape the employer and employee customer experience.
c. Group carriers traditionally have often been reluctant to make significant investments in technology and when they have, they’ve attempted to build new technology solutions in-house. However, with the exponential growth of insurtech and the maturation of group-focused core technology, some carriers are finding it both necessary and easier to acquire new solutions rather than build them. Consequently, group insurers are accelerating their investment in core areas, including enrollment, policy administration, and claims, thereby allowing them to improve in a number of areas from quote to close ratios, and from employee program participation to claims management.
Group insurers will continue to build digital & data architecture and expand analytic capabilities
Artificial intelligence, predictive analytics, behavioral economics,
machine learning, robotic process automation, among other technological developments, represent opportunities for group insurers to better understand, acquire, serve and retain customers in new and more cost effective ways.
Carriers are choosing to invest in new digital capabilities to improve customer and channel segmentation and experience, as well as enhance their ability to acquire and retain the right customers. This helps carriers anticipate employer needs and enables solutions to change as employers do. It also promotes better carrier understand of employees’ broader needs beyond the employer relationship.
Also of note, group insurers have long had a significant amount of data and in recent years have taken advantage of advances in big data, reduced cost of computing power, and commoditized analytic techniques to increase their use of data for decision-making and insight generation. However, many of the advances in data have still not translated to improvements in employee level data across the value chain.
See also: Group Insurance: On the Path to Maturity
New investments in data will help group carriers 1) Improve the data architecture that is critical to improving workflow and customer experiences, 2) Focus on employee level data to better meet the needs of employees – especially in the areas of portability, and 3) Incorporate third-party and unstructured data with employee level data, which will help them be more consultative with employers about the design of responses to employee needs.
Implications
Group insurers will increasingly respond to increased absence management needs, even for down market clients
Absence and leave management services are a core service in the disability market and demand is growing.
There has been a spike in requests by employers for absence and leave services as a result of:
a. The January 1, 2018 New York Paid Family Leave Law, which is the most significant paid leave program in the US;
b. Recent localized laws, such as the Paid Sick Leave Ordinance (PSLO) and Paid Parental Leave Ordinance, have increased the local complexity of employer leave and absence tracking; and
c. Increased cross-selling of disability, FMLA, and voluntary products makes the need for claims/absence integrated services more relevant.
In response to these changes, carriers are increasingly adding absence services and platforms to their repertoire. For those familiar with disability, FMLA, and other products, absence is not new. For those who aren’t, tracking the high number of federal, state, and local laws is a tremendous value-add to their client base. In order to improve customer service, carriers are integrating claims and absence into an “event” experience to radically reduce the burden of correspondence that explains payments and absence rights.
M&A activity and insurtech investment will continue to shape in the group market
Moving upstream and downstream among employer segments requires new capabilities.
The traditional way of doing business will not meet changing employer and employee expectations. As a result, M&A, insurtech investment, and maturing group technology solutions will continue to influence the group market in three ways:
a. In addition to the M&A activity we previously noted, there have been other transactions in the group space, including Meiji’s acquisition of Stancorp and Sumitomo Life’s acquisition of Symetra. Acquisitions like these potentially provide much needed capital investment for group players looking to take advantage of the convergence in the space and the opportunity to profitably expand across traditional market segments. This in turn could raise the bar for existing players, especially in areas where they need i) broker or consultant customers to recommend their products, and ii) to address employer needs to respond the changing employer- employee dynamic.
b. There also have been deals adjacent to group benefits, such as CVS’s acquisition of Aetna and the Amazon, Berkshire and JP Morgan joint venture. These developments may impact more than product solutions, pricing and omni-channel distribution and service; they also could significantly reshape the employer and employee customer experience.
c. Group carriers traditionally have often been reluctant to make significant investments in technology and when they have, they’ve attempted to build new technology solutions in-house. However, with the exponential growth of insurtech and the maturation of group-focused core technology, some carriers are finding it both necessary and easier to acquire new solutions rather than build them. Consequently, group insurers are accelerating their investment in core areas, including enrollment, policy administration, and claims, thereby allowing them to improve in a number of areas from quote to close ratios, and from employee program participation to claims management.
Group insurers will continue to build digital & data architecture and expand analytic capabilities
Artificial intelligence, predictive analytics, behavioral economics,
machine learning, robotic process automation, among other technological developments, represent opportunities for group insurers to better understand, acquire, serve and retain customers in new and more cost effective ways.
Carriers are choosing to invest in new digital capabilities to improve customer and channel segmentation and experience, as well as enhance their ability to acquire and retain the right customers. This helps carriers anticipate employer needs and enables solutions to change as employers do. It also promotes better carrier understand of employees’ broader needs beyond the employer relationship.
Also of note, group insurers have long had a significant amount of data and in recent years have taken advantage of advances in big data, reduced cost of computing power, and commoditized analytic techniques to increase their use of data for decision-making and insight generation. However, many of the advances in data have still not translated to improvements in employee level data across the value chain.
See also: Group Insurance: On the Path to Maturity
New investments in data will help group carriers 1) Improve the data architecture that is critical to improving workflow and customer experiences, 2) Focus on employee level data to better meet the needs of employees – especially in the areas of portability, and 3) Incorporate third-party and unstructured data with employee level data, which will help them be more consultative with employers about the design of responses to employee needs.
Implications