 The third punchline is that UPMC didn’t “plausibility-test” its results by seeing if wellness-sensitive medical events – like heart attacks -- declined for the population over the period. Most companies that don’t do this analysis, like Pepsico, say that they didn’t track wellness-sensitive medical events because they didn’t have access to the event rate data. But obviously UPMC had plenty of access to this event information – it is self-insured by a health plan that it itself owns.
All three of those mistakes are inexcusable in light of the fact that, by this point, everybody knows that you need to address them all to show valid results.
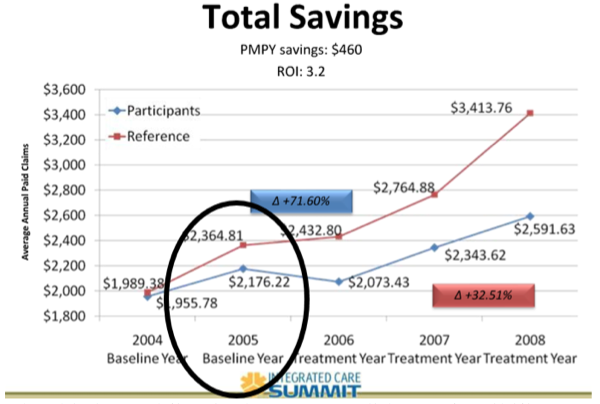
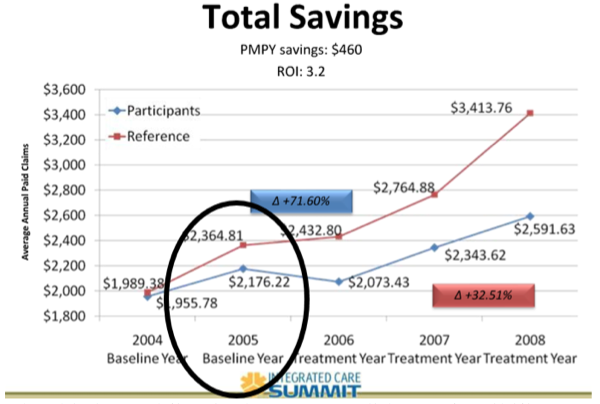
Savings: Also About Nothing
Of course, UPMC also claimed to show substantial savings – who doesn’t? But the savings – according to UPMC's own article – could not have been because of the wellness program. The only three preventive care services that the participants consumed more of than non-participants were checkups, colon cancer screens and breast cancer screens. Checkups have no clinical value, cost money and on balance may be slightly more likely to do harm than good. The intervals and start points for both colon and breast cancer screens have both been relaxed since this UPMC study was performed (2008 to 2011), because doing fewer was deemed by the U.S. Preventive Services Task Force to be a healthier idea than doing more, because of lack of efficacy and overdiagnosis/overtreatment potential and (in the case of colonoscopies) a risk of complications. In any event, whatever money screens save would be years off, as the idea is to find tumors early and spend the money now rather than later. So, screening people does not generate short-term savings and in fact costs money in the short term.
Bottom line: This study did nothing – there is no credible source to attribute savings to, no appreciable risk reduction and lots of liberties taken in study design, and the most important analysis (for plausibility) was conveniently overlooked. Why did UMC even publish this, knowing that it was meaningless? Simple -- UPMC sells this stuff…and it is hoping your western Pennsylvania counterparts will sell it for them, using code language to make sure brokers know that sales come with commissions.
Like every other wellness vendor, UPMC is hoping to entice you with those commissions. Like every other vendor, UPMC gives you a talking point, in this case a conclusion helpfully summarized on the first page, that “wellness programs are a useful tool in managing health and costs.”
Yes, these programs carry commissions, and, no, they are not subject to the same commission disclosure requirements that you must make when selling health plan services. But if you’ve read this far into this posting it’s because you want to do what’s best for your clients, even if it means forgoing short-term commissions. In the long run, you are doing your clients much more good – and, not coincidentally, increasing your chances of keeping those clients – by selling them only the products that are best for them, a list of products that does not include workplace wellness overscreening programs like this one.
The third punchline is that UPMC didn’t “plausibility-test” its results by seeing if wellness-sensitive medical events – like heart attacks -- declined for the population over the period. Most companies that don’t do this analysis, like Pepsico, say that they didn’t track wellness-sensitive medical events because they didn’t have access to the event rate data. But obviously UPMC had plenty of access to this event information – it is self-insured by a health plan that it itself owns.
All three of those mistakes are inexcusable in light of the fact that, by this point, everybody knows that you need to address them all to show valid results.
Savings: Also About Nothing
Of course, UPMC also claimed to show substantial savings – who doesn’t? But the savings – according to UPMC's own article – could not have been because of the wellness program. The only three preventive care services that the participants consumed more of than non-participants were checkups, colon cancer screens and breast cancer screens. Checkups have no clinical value, cost money and on balance may be slightly more likely to do harm than good. The intervals and start points for both colon and breast cancer screens have both been relaxed since this UPMC study was performed (2008 to 2011), because doing fewer was deemed by the U.S. Preventive Services Task Force to be a healthier idea than doing more, because of lack of efficacy and overdiagnosis/overtreatment potential and (in the case of colonoscopies) a risk of complications. In any event, whatever money screens save would be years off, as the idea is to find tumors early and spend the money now rather than later. So, screening people does not generate short-term savings and in fact costs money in the short term.
Bottom line: This study did nothing – there is no credible source to attribute savings to, no appreciable risk reduction and lots of liberties taken in study design, and the most important analysis (for plausibility) was conveniently overlooked. Why did UMC even publish this, knowing that it was meaningless? Simple -- UPMC sells this stuff…and it is hoping your western Pennsylvania counterparts will sell it for them, using code language to make sure brokers know that sales come with commissions.
Like every other wellness vendor, UPMC is hoping to entice you with those commissions. Like every other vendor, UPMC gives you a talking point, in this case a conclusion helpfully summarized on the first page, that “wellness programs are a useful tool in managing health and costs.”
Yes, these programs carry commissions, and, no, they are not subject to the same commission disclosure requirements that you must make when selling health plan services. But if you’ve read this far into this posting it’s because you want to do what’s best for your clients, even if it means forgoing short-term commissions. In the long run, you are doing your clients much more good – and, not coincidentally, increasing your chances of keeping those clients – by selling them only the products that are best for them, a list of products that does not include workplace wellness overscreening programs like this one.UPMC Wellness Plan Meets Seinfeld: It’s About Nothing
The published study is a series of punchlines -- but they aren't funny.

 The third punchline is that UPMC didn’t “plausibility-test” its results by seeing if wellness-sensitive medical events – like heart attacks -- declined for the population over the period. Most companies that don’t do this analysis, like Pepsico, say that they didn’t track wellness-sensitive medical events because they didn’t have access to the event rate data. But obviously UPMC had plenty of access to this event information – it is self-insured by a health plan that it itself owns.
All three of those mistakes are inexcusable in light of the fact that, by this point, everybody knows that you need to address them all to show valid results.
Savings: Also About Nothing
Of course, UPMC also claimed to show substantial savings – who doesn’t? But the savings – according to UPMC's own article – could not have been because of the wellness program. The only three preventive care services that the participants consumed more of than non-participants were checkups, colon cancer screens and breast cancer screens. Checkups have no clinical value, cost money and on balance may be slightly more likely to do harm than good. The intervals and start points for both colon and breast cancer screens have both been relaxed since this UPMC study was performed (2008 to 2011), because doing fewer was deemed by the U.S. Preventive Services Task Force to be a healthier idea than doing more, because of lack of efficacy and overdiagnosis/overtreatment potential and (in the case of colonoscopies) a risk of complications. In any event, whatever money screens save would be years off, as the idea is to find tumors early and spend the money now rather than later. So, screening people does not generate short-term savings and in fact costs money in the short term.
Bottom line: This study did nothing – there is no credible source to attribute savings to, no appreciable risk reduction and lots of liberties taken in study design, and the most important analysis (for plausibility) was conveniently overlooked. Why did UMC even publish this, knowing that it was meaningless? Simple -- UPMC sells this stuff…and it is hoping your western Pennsylvania counterparts will sell it for them, using code language to make sure brokers know that sales come with commissions.
Like every other wellness vendor, UPMC is hoping to entice you with those commissions. Like every other vendor, UPMC gives you a talking point, in this case a conclusion helpfully summarized on the first page, that “wellness programs are a useful tool in managing health and costs.”
Yes, these programs carry commissions, and, no, they are not subject to the same commission disclosure requirements that you must make when selling health plan services. But if you’ve read this far into this posting it’s because you want to do what’s best for your clients, even if it means forgoing short-term commissions. In the long run, you are doing your clients much more good – and, not coincidentally, increasing your chances of keeping those clients – by selling them only the products that are best for them, a list of products that does not include workplace wellness overscreening programs like this one.
The third punchline is that UPMC didn’t “plausibility-test” its results by seeing if wellness-sensitive medical events – like heart attacks -- declined for the population over the period. Most companies that don’t do this analysis, like Pepsico, say that they didn’t track wellness-sensitive medical events because they didn’t have access to the event rate data. But obviously UPMC had plenty of access to this event information – it is self-insured by a health plan that it itself owns.
All three of those mistakes are inexcusable in light of the fact that, by this point, everybody knows that you need to address them all to show valid results.
Savings: Also About Nothing
Of course, UPMC also claimed to show substantial savings – who doesn’t? But the savings – according to UPMC's own article – could not have been because of the wellness program. The only three preventive care services that the participants consumed more of than non-participants were checkups, colon cancer screens and breast cancer screens. Checkups have no clinical value, cost money and on balance may be slightly more likely to do harm than good. The intervals and start points for both colon and breast cancer screens have both been relaxed since this UPMC study was performed (2008 to 2011), because doing fewer was deemed by the U.S. Preventive Services Task Force to be a healthier idea than doing more, because of lack of efficacy and overdiagnosis/overtreatment potential and (in the case of colonoscopies) a risk of complications. In any event, whatever money screens save would be years off, as the idea is to find tumors early and spend the money now rather than later. So, screening people does not generate short-term savings and in fact costs money in the short term.
Bottom line: This study did nothing – there is no credible source to attribute savings to, no appreciable risk reduction and lots of liberties taken in study design, and the most important analysis (for plausibility) was conveniently overlooked. Why did UMC even publish this, knowing that it was meaningless? Simple -- UPMC sells this stuff…and it is hoping your western Pennsylvania counterparts will sell it for them, using code language to make sure brokers know that sales come with commissions.
Like every other wellness vendor, UPMC is hoping to entice you with those commissions. Like every other vendor, UPMC gives you a talking point, in this case a conclusion helpfully summarized on the first page, that “wellness programs are a useful tool in managing health and costs.”
Yes, these programs carry commissions, and, no, they are not subject to the same commission disclosure requirements that you must make when selling health plan services. But if you’ve read this far into this posting it’s because you want to do what’s best for your clients, even if it means forgoing short-term commissions. In the long run, you are doing your clients much more good – and, not coincidentally, increasing your chances of keeping those clients – by selling them only the products that are best for them, a list of products that does not include workplace wellness overscreening programs like this one.






