I’m the founder and CEO of
WorkersCompensationOptions.com (WCO), a company dedicated to workers’ compensation (WC) and its legal alternatives. This letter is intended to quell the concerns of employees in our client companies—employees who may have been distressed by the recent (mostly negative) publicity from
ProPublica and
NPR regarding options to WC in Texas and Oklahoma.
In case you only saw one installment from the
Insult to Injury series, I’ll provide a quick summary. In 2014, the project's authors started to assimilate massive amounts of data from their research concerning each state’s (and the federal government’s) WC system. In March 2015, the authors began releasing articles with an indisputable premise: Collectively, these systems need improvement.
That commendable beginning eventually gave way, however, to a hypothesis that is supported neither by reality nor by the overwhelming quantity of data the authors provide. Their conclusion (that employers are in cahoots with insurers to pressure attorneys, anonymous doctors and legislators into discarding the lives of an unfortunate few for the sake of bolstering corporate profits) completely misses the mark in pinpointing why so many WC systems are broken beyond repair. In fact, attorneys and doctors put at least as much pressure on WC systems as insurers, and any attempt to depict the medical and legal communities as innocent bystanders in the WC feud is simply too naive to be taken seriously.
[1] I do not doubt the authors’ sincerity in addressing a serious societal problem, but I also do not believe they are equipped to understand the problem they sought—however earnestly—to demystify for their readers. Worse yet, I fear they have positioned themselves in the WC space in a manner that is only likely to retard the implementation of practical solutions.
This letter is prompted by the article on Oct. 14, 2015, which painted an inaccurate—even an irresponsible—picture of both Texas nonsubscription (TXNS) and the Oklahoma option (OKO). As that article’s title (
“Inside Corporate America’s Campaign to Ditch Workers’ Comp”) is lengthy, I’ll shorten it to CDWC going forward.
Texas Nonsubscribing Employees: What Can We Learn?
Texas is exceptional in the WC world because it has, for more than a century, offered employers a viable alternative to WC. Of approximately 380,000 employers in Texas, roughly two-thirds subscribe to a traditional WC system; the other third are nonsubscribers who develop their own models. That’s about 120,000 different systems, and there is plenty to be learned. We’ve seen various organically grown components develop from these disparate systems, many of which superficially resemble WC. Despite those similarities, however, industry experts understand how counterproductive it is to make unilateral comparisons between TXNS and WC.
The authors of CDWC didn’t get that memo.
Of all the various lessons learned from diverse TXNS models, one runs counter to conventional WC dogma: Employers can protect themselves while delivering superior care for employees at a fraction of the cost of WC. Eliminating the inflated costs associated with abusive practices that run rampant in WC is a critical component of that particular lesson.
Because the CDWC authors insist on judging TXNS through the lens of WC, TXNS looks to them like a system that would appeal to skinflint employers who simply do not care whether their employees get hurt. However, because employees of nonsubscribing companies can sue their employers for
tort, the decision to opt out of WC is likely to be penny-wise and pound-foolish for employers who do not take measures to ensure the safety of employees. The CDWC authors’ failure to unpack the importance of tort negligence means many readers will come away from the article without understanding that a typical $50,000 payout in WC could easily be either $0 or $5 million in TXNS—depending on who is at fault for the accident. Even more disappointing is CDWC’s attempt, in a one-sentence paragraph, to gloss over one of WC’s most dangerous shortcomings: the extent to which the no-fault arrangement between employers and employees has removed incentives for safety in the workplace throughout the country.
If you are an employee of one of our Texas nonsubscribers, rest assured that your employer has every reason to minimize workplace accidents and to take very good care of you if an occupational injury occurs.
In a nutshell, your interests are aligned with your employer’s—another critical lesson we’ve learned from TXNS.
Oklahoma Option Employees: A Whack-a-Mole WC System Led You Here
ProPublica and NPR harp on a consistent theme throughout the
Insult to Injury series: WC is broken. We at WCO agree, and Oklahoma may provide the single best example of how and why a state’s WC system becomes unsustainable.
The WC ecosystem is made up of five major communities: insurance, medical, legal, employer and employee. Abuse within the system by any of these communities leads to adjustments to the boundaries of the system. Throughout the
Insult to Injury series, the authors go out of their way to sidestep the discussion of systemic abuse. They even attempt to dismiss fraud by citing a study that minimizes its role. Abuse and fraud in WC are, in some ways, analogous to speeding on the highway: Almost all drivers abuse the speed limit, but very few are issued citations. Similarly, the cases of clear-cut fraud in WC only reflect a small portion of the amount of abuse going on. But even if we allow the authors to exclude all instances of clear-cut fraud from the WC conversation, we are still left with rampant abuse driven by insidious systemic incentives.
For decades, abuses and inefficiencies within the WC system have led to each of the five communities touting the need for major reforms—at the others’ expense. Real reform threatens each community, which leads to stalemates in negotiations. Major upheaval has been avoided via the compromise of pushing and pulling the system’s boundaries, resulting in a decades-long game of whack-a-mole being played across the nation. If one voice cries, “
Data shows an
alarming trend in opioid abuse,” that mole gets swatted by
requiring more medical credentials for prescribing pain killers. When another shrieks, “Overutilization is surging,” that mole is whacked through costly and time-consuming independent medical examinations. When someone else observes, “Our disability payouts are higher than neighboring jurisdictions,” that mole prompts us to lower disability payouts. Immediately, a fourth voice shouts, “
Pharmaceutical abuses make up 8.4% of total costs,” and that mole persuades us to introduce drug formularies. But there isn’t even a moment of silence before another voice remarks, “Our analysis shows dismemberment payouts in this jurisdiction are lower than those of our neighboring jurisdiction.” That mole gets whacked by
proposing legislation to increase dismemberment payouts—legislation that is
dead on arrival.
[2] At some point, we have to realize the moles are multiplying faster than we can whack them. (If my commentary doesn’t apply to other jurisdictions, I’m happy to restrict it to Oklahoma and Texas because writers can best serve their readers by acknowledging the limitations of their own expertise.)
Even if we concede that the changes detailed in the paragraph above aren’t necessarily bad (which I’m not conceding; I’m just trying to be polite and move the argument along), they demonstrate a persistent pattern of outcomes, inclusive of abuse, inherent in any hierarchical bureaucratic system. Regulators are busy reacting to entrenched abuses while market participants find new and exciting ways to game the system. This futile game of whack-a-mole is endless.
The Sooner State had a front row seat to witness what TXNS accomplished—both the good and the bad.
[3] With that first-hand knowledge, the Oklahoma legislature has finally provided the state—
and the country—with an opportunity to see whether
real change can restore function to a malfunctioning system. While WC stakeholders assure us they are only a few more whacks-at-the-mole away from making WC hum, Oklahoma lawmakers have written a new chapter in the history of workplace accident legislation. The OKO is neither WC nor TXNS.
The brilliance of the OKO is that it doesn’t attempt to overhaul a broken WC system. The legislators effectively stepped away from that decades-old stalemate. Instead of an all-out overthrow, they left WC in place and created an option for employers who were willing to try something new—which is exactly how WC itself was introduced a century ago.
Because the OKO is substantially modeled on TXNS, it is easy to see why the CDWC writers conflated the two in their analysis. The errors in CDWC concerning
ERISA’s applicability, employee benefits and appeals committee processes in Oklahoma are all presumably honest mistakes made by writers who, in their zeal to distinguish TXNS and the OKO from WC, failed to distinguish TXNS and the OKO from each other.
Nevertheless, it’s important for employees to understand that TXNS varies dramatically from one employer to another, and many of the rules concerning TXNS do not apply north of the Red River.
Although the CDWC authors misleadingly couple TXNS and the OKO with respect to ERISA’s applicability, ERISA plays no direct role in occupational accidents in the OKO.
[4] We’ll be happy to get you a legal opinion on that, but for our purposes regarding CDWC, take my non-legal opinion as on the record. If others disagree, they should go on the record, as well. While ERISA has served employers and employees well in TXNS, its role in the OKO is only implied (if that). We are free to use it where we wish, as long as we are compliant at the state level.
Presumably tied to their ERISA misapplication, the CDWC authors assert that “benefits under opt-out plans are subject to income and payroll taxes.” Such tax advice is unusual from investigative journalists without citation, and I have asked the authors to share their source. Although the jury is still out on this tax issue, it is a point the CDWC authors must distort to substantiate their otherwise baffling claim that the workplace accident plans of OKO employers “almost universally have lower benefits.”
[5] If any OKO plans really do offer benefits that aren’t at least as good as those provided by WC, they’re illegal. That’s how the legislators have written the law, and it’s what they’re dedicated to achieving for workers, regardless of obfuscations invoking TXNS, ERISA and unresolved tax implications.
The authors of CDWC also completely misrepresent appeals committees for at least a majority of OKO employers. The authors overlook a dramatic improvement to employee protection that the OKO makes to TXNS when they claim that appeals committees in Oklahoma work analogously to appeals committees in Texas: “Workers must accept whatever is offered or lose all benefits. If they wish to appeal, they can—to a committee set up by their employers.” That’s dead wrong. Executives at each of our OKO employers are fully aware that, in case of an employee appeal, the employer has nothing to do with the selection of the appeals committee panel members or the work they complete. The process is
independent from the employer and extremely fair.
[6] The CDWC authors would do well to read Section 211 of the law more carefully.
On the subject of benefit denials, I’ll share a single data point from our OKO book: To date, we have denied exactly one claim. This is a nascent system, so we must be very careful in drawing actuarial conclusions. Still, our company has led more employers from traditional WC into the new OKO than any other retailer, so we have a bit of credibility to offer on this subject. The point of the system isn’t to deny benefits to deserving employees but to ensure benefits are delivered more efficiently. The system is working.
The CDWC authors only provide one OKO case study, Rachel Jenkins. Strangely, they lump Jenkins in with four TXNS case studies. The Jenkins
case is still being tried. We will withhold opinions—as we hope others would—until a more appropriate time.
As a reminder, while the OKO law is stronger today than ever, if it were to be deemed unconstitutional by the Oklahoma Supreme Court, we would have 90 days to get everyone back into traditional WC (per
Section 213.B.4.).
Next: Vigilance and Diligence
My comments are mine and mine alone. I do not speak for any associations or lobbyists. I have no interest in debating those who inexplicably assume that any alternatives proposed to a failing system must stem from sinister motives. However, I encourage anyone (from prospective clients to employees of existing clients) with questions or concerns to call me.
Another option for learning more is to
click here and watch a formal debate regarding the OKO. This footage was shot in September 2015. It features
Michael Clingman arguing against the OKO while I, predictably, argue for it. One thing you can’t miss in that video is my desire to oust most attorneys from the scene. To help explain, I’ll
adapt a quotation from John F. Kennedy (who was discussing taxation) to my own area of concern (the well-being of employees): “In short, it is a paradoxical truth that employee outcomes from increased WC protections are worse today, while economic results suffer, and the soundest way to create higher and better standards of living for employees is to eliminate these abused protections.” For philosopher kings, the theory of the OKO may not sound as good as the theory of WC, but when it comes to practical realities the results demand everyone’s attention.
To summarize my primary criticism of
Insult to Injury, it simply hasn’t done enough. The story it tells is insufficient and smacks of partisanship and ideology, two
biases that ProPublica’s journalists allegedly avoid. WC is substantially more complex than a corporation-out-to-exploit-its-workforce short story. Ignoring abuse in each of the communities in a five-sided WC debate demonstrates a lack of journalistic impartiality and a stunning deficiency of perception. Moreover, to my knowledge, ProPublica hasn’t crafted any relevant suggestions for legislation, simply leaving its readers with the vague and implicit notion that federal oversight is needed. If that is the goal of
Insult to Injury—to provide one-sided, emotional yarns alongside a treasure trove of data, hoping it will all spur
some federally elected officials to create real change at long last—then I suspect ProPublica will still be holding this subject up to the light of opprobrium upon the retirement of each of the series’ authors.
We do not aspire to win over the authors or even their followers. We will focus our energies each day on providing the best workplace accident programs for employers and employees alike. Our results should speak for themselves.
Finally, I am not an attorney, and nothing in this letter should be taken as legal advice.
Sincere regards,
Daryl Davis
Footnotes:
[1] With medical providers, overutilization is always a concern.
Click here and watch the video from the 12-minute to the 15-minute mark for a detailed description of rampant WC abuse by surgeons who provide unnecessary and damaging back procedures. If the workers weren’t disabled prior to the surgeries, many were afterward. As for the legal community, simply view slide 73 of the
NCCI’s 2013 Oklahoma Advisory Forum. WC disability payments, which is where attorneys get their cut, were 38% higher in Oklahoma than in neighboring states—not because jobs are 38% more dangerous in Oklahoma than in Kansas or Texas but because Oklahoma attorneys are 38% more effective at gaming the state’s WC system.
[2]
Alabama SB 330—which was
prompted by
Insult to Injury—
never got out of conference. From what I could gather, lengthy negotiations between several different interest groups led nowhere, with the Alabama Medical Association at the center of this particular stalemate. Not surprisingly,
the two special sessions called by Alabama Gov. Bentley in 2015 were strictly focused on the state’s
budgetary crisis; this bill was never discussed.
[3] The final Texas case study offered in CDWC deals with Billy Walker, who fell to his death while on the job. The upside to TXNS is his estate’s common law right to pursue a tort lawsuit against his employer. The employer could have been ordered to pay Walker’s estate a settlement in the millions, but the employer filed bankruptcy before any such judgment could be awarded, which is plainly an unacceptable outcome. This demonstrates a lack of surety—the single biggest problem in TXNS. OKO addresses this issue in various ways, most notably in
Section 205 of Title 85A, which guarantees surety for injured workers.
[4] For the non-occupational components of your OKO program, ERISA does apply.
[5] Per Section 203.B. of the statute, compliant plans “shall provide for payment of the same forms of benefits included in the Administrative Workers' Compensation Act for temporary total disability; temporary partial disability; permanent partial disability; vocational rehabilitation; permanent total disability; disfigurement; amputation or permanent total loss of use of a scheduled member; death; and medical benefits as a result of an occupational injury, on a no-fault basis, with the same statute of limitations, and with dollar, percentage and duration limits that are
at least equal to or greater than the dollar, percentage and duration limits contained in Sections 45, 46 and 47 of this act.” (Emphasis mine.)
[6] Details of OKO appeals committee procedures are generally misunderstood—for now—by plaintiffs’ attorneys (and, apparently, investigative journalists). Attorneys frequently assume that, because the employer foots the bill, the employer controls the process. For a peek at how the appeals committee process really works for a majority of OKO employers, those curious should
watch this video.
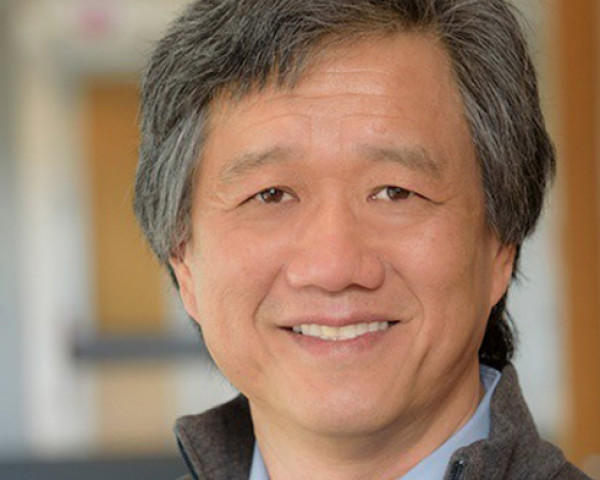
 Craig Spiezle, Online Trust Alliance executive director
Craig Spiezle, executive director of Online Trust Alliance, says some of the vulnerabilities, such as unsecure sites, are obvious to the casual person, let alone criminals.
“These sites are such high targets, you’d expect 100% of these to be like Fort Knox,” he says. “There’s no perfect security, but you would expect not to see (simple) vulnerabilities.”
Some e-filing sites, for example, had simple server misconfigurations or didn’t have current secure protocols; one provider failed to adopt an extended validation (EV) SSL certificate, leaving it open to spoofing.
Although not everyone is eligible for the free e-filing services that OTA audited, Spiezle says many of the paid e-filing services are run by some of the same parent companies, and thus use much of the same lightly protected infrastructure. He says it would be fair to assume that many of the paid e-filing sites would have the same 46% failure rate as the free e-filing services audited by OTA.
Personal information trades on black market
Even if cyber criminals don’t use stolen tax-related data for filing fraudulent returns, that information is highly valuable on the black market. Spiezle points out that it’s the only place where this type of rich information—such as income, employer, number of dependents, Social Security numbers and even bank accounts—is available all in one swoop.
“All that data that’s amassed is a treasure chest,” he says. “If you want to create a persona of someone’s identity, you have all the data in one place.”
The IRS expects that, this year, 80% of the estimated 150 million individual tax returns will be prepared with tax software and e-filed—and that’s music to fraudsters’ ears.
One typical avenue for cyber thieves is to file returns as early as possible, claiming refunds as large as $1,000 to $4,000 on untraceable prepaid debit cards. They can fly under the radar by filing very generic returns, and those multiple refunds turn into a lucrative operation.
“They have immediate access to that cash, as opposed to credit card fraud where the value is not as high and the delivery is through a retailer, so they have to figure out what to do with those goods,” says Scott Olson, vice president of product at iovation, a provider of device authentication and mobile security solutions.
Phishing, malware skyrocket
According to the Government Accountability Office, the IRS prevented $24 billion in fraudulent tax refunds related to identity theft in 2013, while paying out $5.8 billion in fraudulent refunds that it didn’t discover until a year later. And the number of fraud attempts is on the rise: As of March 25, the IRS reported a 400% increase in phishing and malware incidents related to the 2016 tax season.
Email phishing campaigns include links to web pages requesting personal information, useful for filing fake returns.
These fake pages often imitate an official-looking website, such as IRS.gov or an e-filing service, and also may carry malware, which can turn over control of the victim’s computer to the attacker. This January alone, the IRS counted 1,026 email-related fraud incidents, compared with 254 a year earlier.
Phishing scams also are targeting employers—because criminals know that’s where they can find large caches of income-related information. One growing trend is the so-called business email compromise (also known as “CEO fraud”), a variation of spear phishing. The phisher does deep research on a targeted company, then impersonates a senior executive to get a subordinate to do something.
Craig Spiezle, Online Trust Alliance executive director
Craig Spiezle, executive director of Online Trust Alliance, says some of the vulnerabilities, such as unsecure sites, are obvious to the casual person, let alone criminals.
“These sites are such high targets, you’d expect 100% of these to be like Fort Knox,” he says. “There’s no perfect security, but you would expect not to see (simple) vulnerabilities.”
Some e-filing sites, for example, had simple server misconfigurations or didn’t have current secure protocols; one provider failed to adopt an extended validation (EV) SSL certificate, leaving it open to spoofing.
Although not everyone is eligible for the free e-filing services that OTA audited, Spiezle says many of the paid e-filing services are run by some of the same parent companies, and thus use much of the same lightly protected infrastructure. He says it would be fair to assume that many of the paid e-filing sites would have the same 46% failure rate as the free e-filing services audited by OTA.
Personal information trades on black market
Even if cyber criminals don’t use stolen tax-related data for filing fraudulent returns, that information is highly valuable on the black market. Spiezle points out that it’s the only place where this type of rich information—such as income, employer, number of dependents, Social Security numbers and even bank accounts—is available all in one swoop.
“All that data that’s amassed is a treasure chest,” he says. “If you want to create a persona of someone’s identity, you have all the data in one place.”
The IRS expects that, this year, 80% of the estimated 150 million individual tax returns will be prepared with tax software and e-filed—and that’s music to fraudsters’ ears.
One typical avenue for cyber thieves is to file returns as early as possible, claiming refunds as large as $1,000 to $4,000 on untraceable prepaid debit cards. They can fly under the radar by filing very generic returns, and those multiple refunds turn into a lucrative operation.
“They have immediate access to that cash, as opposed to credit card fraud where the value is not as high and the delivery is through a retailer, so they have to figure out what to do with those goods,” says Scott Olson, vice president of product at iovation, a provider of device authentication and mobile security solutions.
Phishing, malware skyrocket
According to the Government Accountability Office, the IRS prevented $24 billion in fraudulent tax refunds related to identity theft in 2013, while paying out $5.8 billion in fraudulent refunds that it didn’t discover until a year later. And the number of fraud attempts is on the rise: As of March 25, the IRS reported a 400% increase in phishing and malware incidents related to the 2016 tax season.
Email phishing campaigns include links to web pages requesting personal information, useful for filing fake returns.
These fake pages often imitate an official-looking website, such as IRS.gov or an e-filing service, and also may carry malware, which can turn over control of the victim’s computer to the attacker. This January alone, the IRS counted 1,026 email-related fraud incidents, compared with 254 a year earlier.
Phishing scams also are targeting employers—because criminals know that’s where they can find large caches of income-related information. One growing trend is the so-called business email compromise (also known as “CEO fraud”), a variation of spear phishing. The phisher does deep research on a targeted company, then impersonates a senior executive to get a subordinate to do something.