Editor’s Note: This is the second in a series of posts in which CJ Lotter, a 15-year industry veteran, shares lessons learned in the form of guidance to MGAs on the steps required to build a successful program. The first post is here.
The trend in insurance today is toward large volumes of policies with very little human intervention. Although the cost benefits may be attractive, this movement is leading us toward a commoditization of the industry where the only differentiator is price. Any business-minded person will tell you this is not a good position to be in.
Ideally, you want to sell unique solutions that are difficult to replicate, raising the barrier to entry. There is an alternative to commodity products. It’s called programs.
The best program business is difficult to understand, labor-intensive and hard to automate. Unique underwriting expertise is required, and it should be hard to find and difficult to train. The role of technology in this market is to assist the process and provide the flexibility to adapt to unique risks, not to replace human ingenuity with mass automation.
For an MGA seeking to launch a new program, there are three types of opportunity that provide the greatest potential: a distressed class, a perceived distressed class and an underserved class.
A distressed class is one that most underwriters don’t understand or for which losses are difficult to predict. To underwrite this business, you need unique underwriting skills – an understanding of the nuances of the class and of the characteristics of the risk that could produce significant losses. Clever underwriting and careful selection of risks is key to remaining profitable in this niche. Heavy loss control may be required here, too. Your ability to make this riskier class safer is your competitive advantage.
See also: 10 Steps to Successful Insurance Program
Nuclear plants are one example of a distressed business class. The dynamics of radioactive materials and the consequences of their incorrect handling are complicated. Losses are catastrophic and will most likely include loss of life, millions of dollars of property losses and loss of business income. Underwriting this class calls for highly trained underwriters who know a good risk from a bad one. These are specialists who can assess, for example, whether safety manuals and procedures are sufficient to minimize the potential for losses.
A perceived distressed class refers to business that potential competitors shy away from because their underwriters perceive it as too risky. By careful analysis, a clever underwriter can discover that what others thought were drivers of claims were indeed not so. Ski resorts are one example of perceived distress. Underwriters may avoid this class because of the downhill ski exposure, while the real claims drivers are slips and falls in the restaurant. This is an extreme example, but it illustrates the point.
The underserved class is another spin on program opportunities. The less competition in a class, the better the chances for a successful program. There are many reasons markets avoid certain classes. It may be that the specific geographic territory is overly litigious or that the universe for this specific class is small. Whatever the reason, once you identify the issue and find a solution or compromise, you will have uncovered a program opportunity with little competition.
The class may also be underserved because a traditional “old school” risk taker with archaic systems is the only alternative for this specific class of risk. By providing modern technology with automation that makes it easy to do business, you can outperform the competition and capture your fair share of the market.
An example of this kind of risk may be trash truck operators in the boroughs of New York City. It’s a tough jurisdiction to write trash hauling insurance. A longtime traditional insurance company may have locked up the market. But at the same time, pricing may have crept up over the years, and customer service and loss control may be stale. There is no meaningful competition in this space, and it’s ripe for the introduction of an MGA program.
Start with an updated product offering that includes new coverages like data destruction and privacy, and dynamic pricing tuned to the characteristics of each individual risk. Round off the offering with quick quote turnaround, killer personalized service and fast and fair claims handling, and you’ve got a program that will attract business from the incumbents.
See also: Is There a Future for MGAs?
So, there you have it – three scenarios that provide the first ingredients for building a new insurance program. Whichever you choose, when you create your program, ask the following question: “Will my program be so different that it will be difficult to duplicate, and so appreciated by buyers that price will not be the focus?” If your answer is “yes,” you have taken the first step to a successful program.
Excerpted with permission from Instec. A complete collection of Instec’s insurance industry insights can be found here.
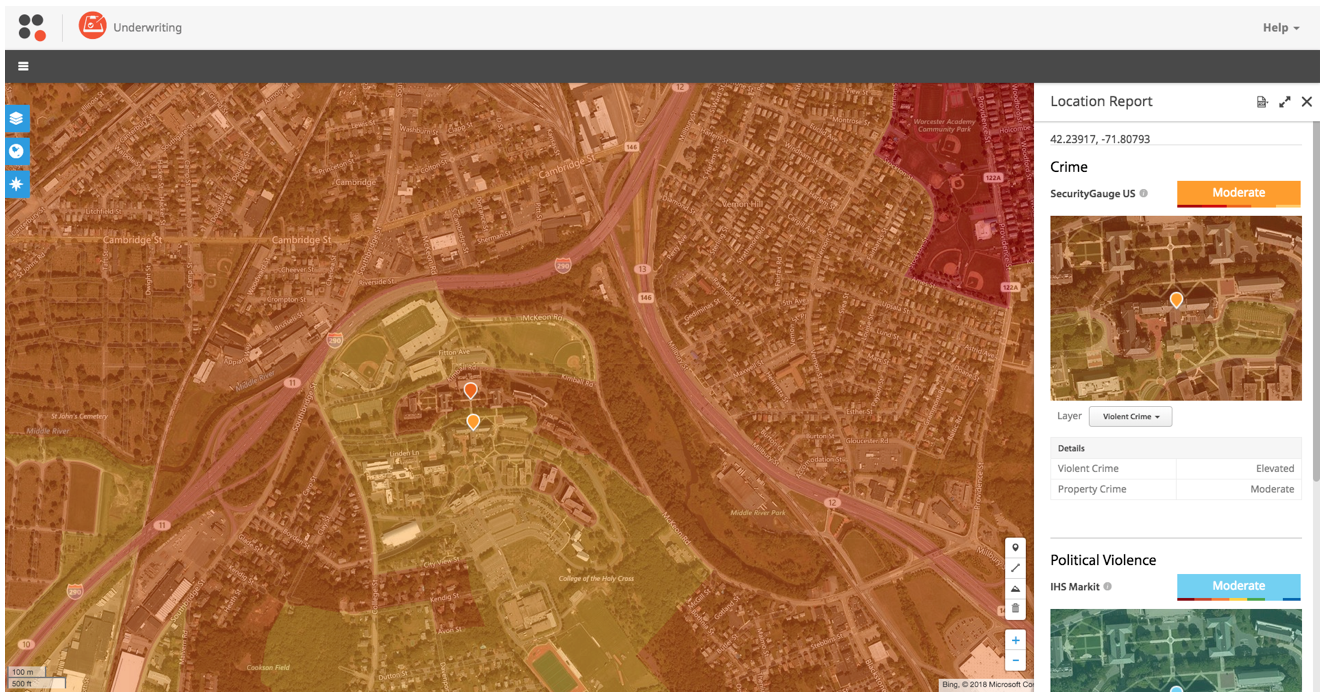 As you can see, there is a clear delineation between the school’s campus (near average risk relative to the nation, shown in yellow) and the surrounding city (in orange/red), which has an elevated crime score. So while the school itself is at or below the national average for crime risk, knowing that there is some high crime nearby could raise a flag to ensure proper coverages and adequate premiums are in place when underwriting this risk.
Use Case 2: Arson
When underwriting property risk outside the U.S. and Canada, for example in the U.K., Pitney Bowes crime data, for England, Wales, Scotland, and Northern Ireland, can be used within SpatialKey to understand factors driving overall risk, as shown below.
As you can see, there is a clear delineation between the school’s campus (near average risk relative to the nation, shown in yellow) and the surrounding city (in orange/red), which has an elevated crime score. So while the school itself is at or below the national average for crime risk, knowing that there is some high crime nearby could raise a flag to ensure proper coverages and adequate premiums are in place when underwriting this risk.
Use Case 2: Arson
When underwriting property risk outside the U.S. and Canada, for example in the U.K., Pitney Bowes crime data, for England, Wales, Scotland, and Northern Ireland, can be used within SpatialKey to understand factors driving overall risk, as shown below.
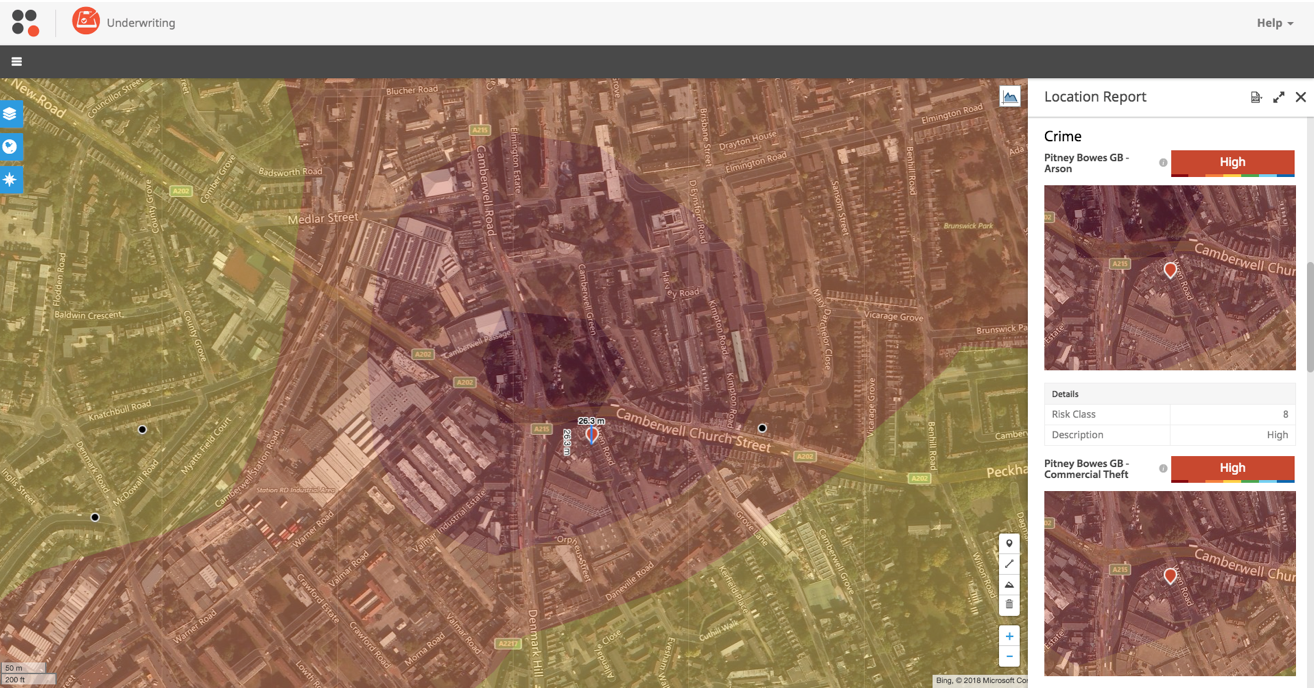 The location has a very high score (borderline extreme, in fact) for arson. When looking at this map, you can see that there is a bus depot across the street from the location in question. This information should factor into your risk assessment due to the flammable nature of the bus depot.
These use cases demonstrate how using expert crime risk data wcan help insurers:
The location has a very high score (borderline extreme, in fact) for arson. When looking at this map, you can see that there is a bus depot across the street from the location in question. This information should factor into your risk assessment due to the flammable nature of the bus depot.
These use cases demonstrate how using expert crime risk data wcan help insurers: