Sufferers of long COVID are often referred to as “long haulers” because symptoms can last for weeks or even months. And it is not just a person’s health that is affected for the long-term; there are many other knock-on impacts of extended symptoms, such as impact on life insurance, that industries will now have to consider and adapt to.
Much remains unknown, but the first step to navigating this new territory, for life insurance is to understand the data we do have so far.
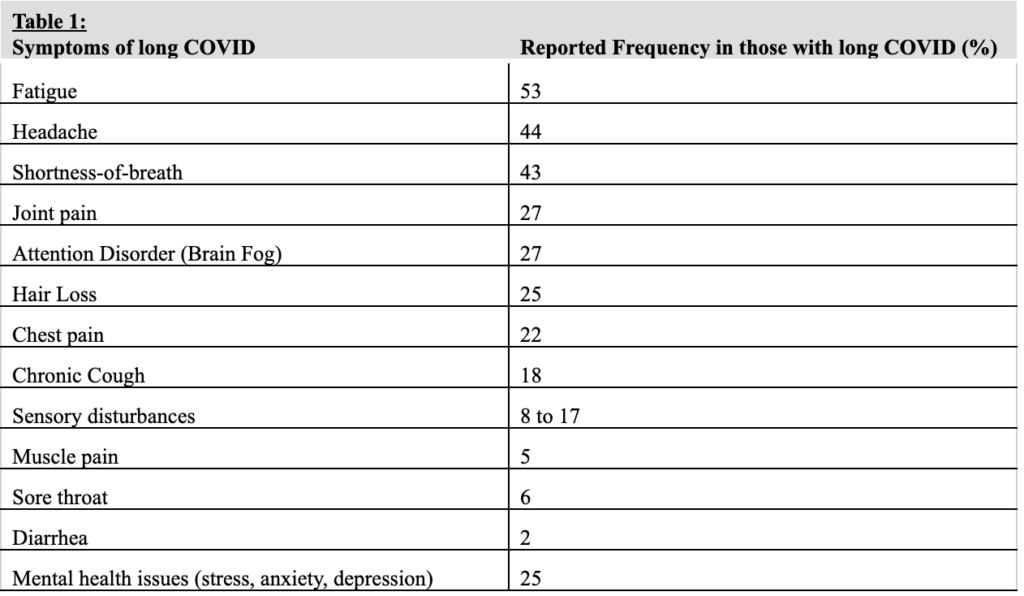
Symptoms of long COVID
What do we know about long COVID?
We know that symptoms — shown in Table 1 below — may occur continuously or in a relapsing pattern. The symptoms may simply persist for a long time following the initial infection of COVID-19, or, over time people may experience new symptoms.
Interestingly, by far the majority of patients with long COVID test negative for the virus, indicating microbiological recovery. As such, the causes of long COVID remain uncertain. Possible explanations include organ damage from the virus, exaggerated immune or autoimmune responses and persistent but undetectable viral reservoir.
Classification of long COVID
Experts have also started to classify long COVID in two different stages. The first, referred to as post-acute COVID, applies to cases where symptoms persist for more than three but less than 12 weeks after the initial infection. The second, called chronic COVID, applies to instances where symptoms persist for more than 12 weeks following initial infection.
Experts also suggest that an alternative way of classifying long COVID is according to the predominant residual symptom experienced. Based on this approach, sufferers can be classified as having post-COVID cardiorespiratory syndrome, meaning likely to suffer with breathing problems; post-COVID fatigue syndrome, meaning likely to feel persistent low energy levels; or post-COVID neuro-psychiatric syndrome, meaning likely to experience cognitive dysfunction such as depression, anxiety or brain fog.
Risk factors for long COVID
What do we know about who is most likely to develop long COVID?
Data suggests that patients hospitalized during the initial COVID-19 infection have an increased risk of developing long COVID (87%) compared with those treated with outpatient COVID-19 (10% to 35%). Hospitalized patients are also more likely to sustain organ damage from their initial infection, leading to prolonged symptoms.
What’s more, the number of symptoms presented at the time of initial infection appears to predict the likelihood of a person developing long COVID. The more symptoms at initial infection, the higher the risk of developing a long COVID syndrome of some kind.
Long COVID is more commonly reported in adults aged 50-plus, although it can occur in any age group, including children.
Individuals with co-morbid disorders, and in particular co-morbid psychiatric disorders, such as depression or anxiety, have an increased risk of developing long COVID after infection. The more co-morbidities, it appears, the higher the risk.
See also: Long-Haul COVID-19 Claims and WC
Long COVID and Morbidity
The link between long COVID and morbidity must be continuously assessed. At this early stage, not enough data exists to provide a clear understanding.
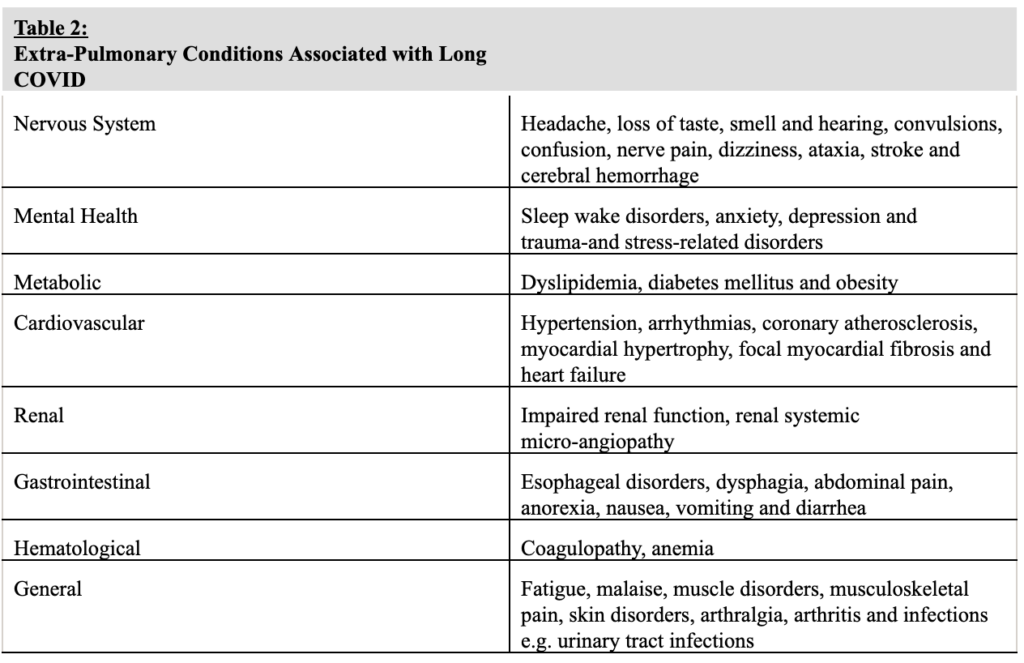
That said, wide varieties of new-onset pulmonary and extra-pulmonary disorders, meaning conditions associated with the lungs, have been observed in long COVID patients, including interstitial lung disease and respiratory failure. Table 2 shows a list of the extra-pulmonary conditions associated with long COVID.
Additionally, according to a recent longitudinal study of more than 73,000 U.S. veterans with a history of outpatient COVID-19 infection, there was an increase in observed short-term mortality at six months, when compared with veterans with no history of COVID-19 infection. However, the picture is far from complete, and more research is required for an accurate understanding of the mortality associations of various long COVID syndromes.
Evaluation of long COVID for life insurance purposes
When it comes to evaluating the associated risks of a person experiencing long COVID, the predominant residual symptom profile should be used to guide the evaluation. For example, if the predominant symptoms presented are shortness of breath and chest pain, cardiorespiratory investigations such as lung function tests, EKG, echo or chest imaging should be conducted.
For more general symptom profiles, blood and imaging tests will need to be conducted, guided by clinical assessment, and may include tests such as complete blood count, liver and renal function analysis, urinalysis, D-dimer assay testing (which screens for clots or deep vein thrombosis), inflammatory marker testing (which evaluates the presence of inflammation) and NT proBNP testing (which detects signs of heart failure).
Underwriting considerations
When it comes to life insurance underwriting, there is some early-stage guidance to help navigate this new territory. One of the most important factors to consider is adjusting ratings in the case of any evidence of organ damage. To date, though, for sufferers of long COVID with no evidence of organ damage, there does not appear to be any significant excess mortality risk to take into account when underwriting.
As with any emerging condition, the picture we have today, and the industry’s understanding of risk, will become a lot clearer in time. What’s needed now is continued study and analysis of patterns so new underwriting rules can be developed. One thing is for sure, though: The COVID-19 virus is leaving a troubling legacy.