A major part of Healthcare Consumerism (HC) is related to stress and depression in the workplace. Stress and depression costs (including co-morbid costs) for U.S. businesses are over $200 billion per year according to a 2015 study by the Journal of Clinical Psychiatry. Recognition of the need for stress management can link healthcare, consumerism, and organizational quality, safety, and error reduction programs. In addition, improved product quality and productivity can result with focused efforts to address areas such as stress and depression in the workplace.
One thing is certain – if an organization does not have a structured stress management program for employees, it is 100% certain that employees will deal with their stress in other ways (e.g. comfort food, alcohol, drugs, smoking, etc.)
U. S. Surgeon General David Satcher once said, “There is no health without mental health.” Similarly, there is no effective program of HC without mental healthcare consumerism. It is a basic requirement for any employer implementing HC plans to deal with stress, depression, and more serious mental illnesses. It is important for employers to understand the clinical and cost inter-relationships between “mind care” and “body care.”
Studies show that stress affects an organization in many ways:
1. Healthcare - 21.5% of total health care costs
2. Turnover - 40% of the primary reasons that employees leave a company
3. Impaired Presenteeism - 50% of impaired presenteeism is a function of stress
4. Disability - 33% of all disability and workers’ compensation costs
5. Unscheduled Sickness - 50% of the primary reasons that employees take unscheduled absence days
To work for everyone, HC must help the sickest and most vulnerable. Mental illnesses present a unique challenge. Depression is a sickness where patients tend to push away care givers. Many with depression and co-existing physical illnesses will deny their need for care, ignore treatment advice, skip appointments, and are highly non-compliant with medications.
A 2014 Kaiser poll showed 48% of employers offer wellness in the workplace. But, a 2013 survey by the
American Psychological Association's Center for Organizational Excellence found that despite growing awareness of the importance of a healthy workplace, fewer than half of employees said their organizations provide sufficient resources to help them manage stress (36 percent) and meet their mental health needs (44 percent).
See also: How to Improve Stress Testing
Stress has a distinct correlation with medical issues in other body systems. Stress Directions, a leading consultancy on stress, found: “44% of all adults suffer adverse health effects from stress; 75 to 90% of all physician office visits are for stress-related ailments and complaints; stress is linked to the 6 leading causes of death - heart disease, cancer, lung ailments, accidents, cirrhosis of the liver, and suicide.”
Stress Directions, Inc. outlines the following relationships:
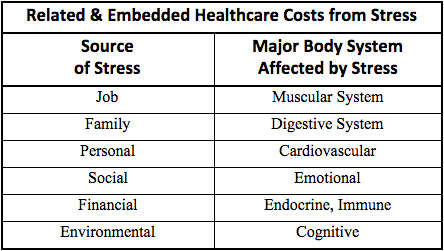
If your plan is not properly dealing with member stress, you will increase the cost of treating the manifestations of stress in those body systems where health costs are covered. These correlations are why well-being is a growing area of interest. Providing support programs for the whole person whether at work or at home will lower health costs and improve productivity.
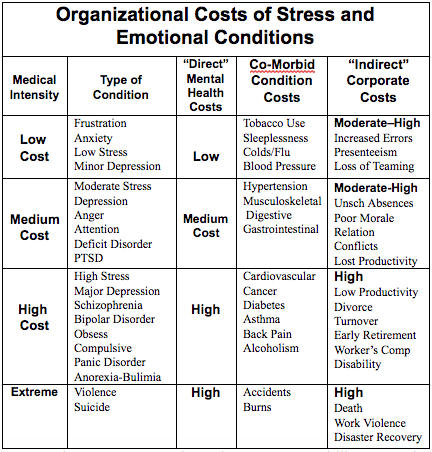
The Occupational Safety and Health Administration (OSHA) has declared stress a "hazard of the workplace.” There are at least three separate, but related costs of stress in the workplace:
1. Direct Mental Health Costs – as separate diagnoses these costs can range from low to high costs.
2. Co-Morbid Condition Costs – many times the more obvious physical health symptoms are treated, but the underlying mental health issue is ignored.
3. Indirect Corporate Costs – these are costs from absenteeism, disability, unscheduled sick days, loss of teaming, relationship conflicts, etc.
With the assistance of many national mental health experts and organizations, Healthcare Visions, Inc. has organized a chart showing the relationships among the three types of corporate costs.
Companies can no longer treat stress, depression, or any mental illness as a single diagnosis. Because of coexisting mental illnesses, many employees will not effectively recover from or stabilize chronic and persistent conditions such as diabetes, asthma, heart conditions, hypertension, or cancer unless an effective stress management program is implemented.
A 2005 study for Dupont Company by the University of Pennsylvania showed that depression, when measured by its impact on total costs (direct and indirect costs), was the highest corporate cost medical condition. The second highest total cost was from musculoskeletal issues that likely also involved stress related costs.
See also: Consumerism: Good, Bad, Future
Medical, clinical, and medication therapies have advanced such that clinical depression and other mental health conditions have cure rates equal to and greater than many medical conditions. Clinical depression can be cured. Treatments work. Medications are effective. No company, large or small, can avoid the costs of depression. Divorce, disability, and violence in the workplace can hit anyone at anytime. According to the Institute of Medicine 30,000 people die each year from suicide, and 90% had diagnosable and treatable depression. For a small employer the results can be devastating if a key employee or executive suffers from clinical depression.
Tom Johnson, former CEO of CNN News, likes to say, “If a company’s computers crashed and corporate production ground to a halt, the CEO would demand immediate action to re-establish the “corporate brains.” In developing a “knowledge-based” workforce, it is just as important for CEOs to take care of mental health and the “central computer” – the brain - within each employee.”
Most employers do not understand the complexities of clinical mental health diagnoses. They do not know what it means to have schizophrenia, a somatoform disorder, a factitious disorder, or get a multi-axial assessment. Tom Johnson understood as he often suffered from serious bouts of clinical depression. Tom has dedicated his life to helping others deal with the debilitating effects of depression.
Case Study
As an actuary and mathematician, I was trained in numbers and actuarial science. Many of you may also be analysts, doctors, lawyers, CEOs, economists, or researchers. Let’s throw away the numbers for a moment and look at the lives of real people.
Let me tell you about a young man, age 30, who suffered multiple inherited physical problems: a blood disorder, clotting concerns, pulmonary hypertension, and other unfathomable sources of pain and suffering. Combined with depression and the stigma of an emotional disorder, this young man was frequently non-compliant with care and treatment. Unlike other physical illnesses, depression typically causes the patient to avoid care. He pushed away the very help that was needed. He pushed away family support and friends that cared.
No young strapping 6’5” 260 pound young man wants his forehead stamped with the stigma of mental illness. He was not going to be classified as “crazy”, see a “shrink”, or go to a “nut house” for care. No, he was a high school basketball star with the athletic promise most boys just dream about. In his mind, he didn’t need care, he was who he was. He didn’t accept or understand chemical imbalances. In his mind, "Real men are strong enough."
In 2005 the years of depression and physical decline took its toll. The death certificate read pulmonary hypertension. But, I can tell you the real cause was stigma and major depression that prevented this young adult from seeking or accepting the medical and life saving care that he needed.
Chris Golden was my step-son. His mother and I buried Chris on May 5, 2005. Look at all the ROI numbers, but never forget. This is not about numbers. It’s about people and saving lives. It’s about the Chris Goldens of the world.
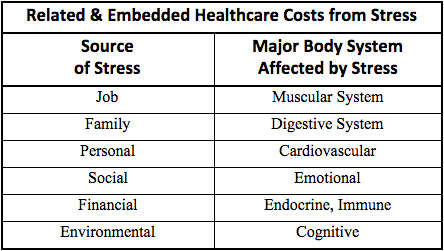 If your plan is not properly dealing with member stress, you will increase the cost of treating the manifestations of stress in those body systems where health costs are covered. These correlations are why well-being is a growing area of interest. Providing support programs for the whole person whether at work or at home will lower health costs and improve productivity.
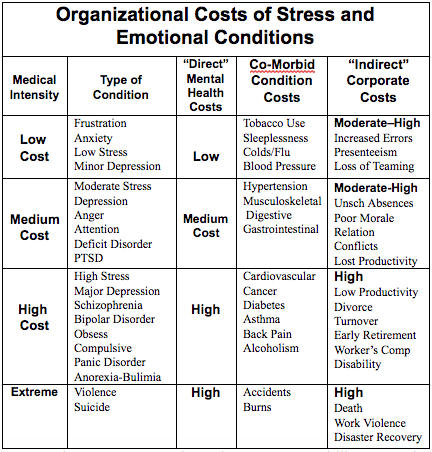
The Occupational Safety and Health Administration (OSHA) has declared stress a "hazard of the workplace.” There are at least three separate, but related costs of stress in the workplace:
1. Direct Mental Health Costs – as separate diagnoses these costs can range from low to high costs.
2. Co-Morbid Condition Costs – many times the more obvious physical health symptoms are treated, but the underlying mental health issue is ignored.
3. Indirect Corporate Costs – these are costs from absenteeism, disability, unscheduled sick days, loss of teaming, relationship conflicts, etc.
With the assistance of many national mental health experts and organizations, Healthcare Visions, Inc. has organized a chart showing the relationships among the three types of corporate costs.
If your plan is not properly dealing with member stress, you will increase the cost of treating the manifestations of stress in those body systems where health costs are covered. These correlations are why well-being is a growing area of interest. Providing support programs for the whole person whether at work or at home will lower health costs and improve productivity.
The Occupational Safety and Health Administration (OSHA) has declared stress a "hazard of the workplace.” There are at least three separate, but related costs of stress in the workplace:
1. Direct Mental Health Costs – as separate diagnoses these costs can range from low to high costs.
2. Co-Morbid Condition Costs – many times the more obvious physical health symptoms are treated, but the underlying mental health issue is ignored.
3. Indirect Corporate Costs – these are costs from absenteeism, disability, unscheduled sick days, loss of teaming, relationship conflicts, etc.
With the assistance of many national mental health experts and organizations, Healthcare Visions, Inc. has organized a chart showing the relationships among the three types of corporate costs.
 Companies can no longer treat stress, depression, or any mental illness as a single diagnosis. Because of coexisting mental illnesses, many employees will not effectively recover from or stabilize chronic and persistent conditions such as diabetes, asthma, heart conditions, hypertension, or cancer unless an effective stress management program is implemented.
A 2005 study for Dupont Company by the University of Pennsylvania showed that depression, when measured by its impact on total costs (direct and indirect costs), was the highest corporate cost medical condition. The second highest total cost was from musculoskeletal issues that likely also involved stress related costs.
See also: Consumerism: Good, Bad, Future
Medical, clinical, and medication therapies have advanced such that clinical depression and other mental health conditions have cure rates equal to and greater than many medical conditions. Clinical depression can be cured. Treatments work. Medications are effective. No company, large or small, can avoid the costs of depression. Divorce, disability, and violence in the workplace can hit anyone at anytime. According to the Institute of Medicine 30,000 people die each year from suicide, and 90% had diagnosable and treatable depression. For a small employer the results can be devastating if a key employee or executive suffers from clinical depression.
Tom Johnson, former CEO of CNN News, likes to say, “If a company’s computers crashed and corporate production ground to a halt, the CEO would demand immediate action to re-establish the “corporate brains.” In developing a “knowledge-based” workforce, it is just as important for CEOs to take care of mental health and the “central computer” – the brain - within each employee.”
Most employers do not understand the complexities of clinical mental health diagnoses. They do not know what it means to have schizophrenia, a somatoform disorder, a factitious disorder, or get a multi-axial assessment. Tom Johnson understood as he often suffered from serious bouts of clinical depression. Tom has dedicated his life to helping others deal with the debilitating effects of depression.
Case Study
As an actuary and mathematician, I was trained in numbers and actuarial science. Many of you may also be analysts, doctors, lawyers, CEOs, economists, or researchers. Let’s throw away the numbers for a moment and look at the lives of real people.
Let me tell you about a young man, age 30, who suffered multiple inherited physical problems: a blood disorder, clotting concerns, pulmonary hypertension, and other unfathomable sources of pain and suffering. Combined with depression and the stigma of an emotional disorder, this young man was frequently non-compliant with care and treatment. Unlike other physical illnesses, depression typically causes the patient to avoid care. He pushed away the very help that was needed. He pushed away family support and friends that cared.
No young strapping 6’5” 260 pound young man wants his forehead stamped with the stigma of mental illness. He was not going to be classified as “crazy”, see a “shrink”, or go to a “nut house” for care. No, he was a high school basketball star with the athletic promise most boys just dream about. In his mind, he didn’t need care, he was who he was. He didn’t accept or understand chemical imbalances. In his mind, "Real men are strong enough."
In 2005 the years of depression and physical decline took its toll. The death certificate read pulmonary hypertension. But, I can tell you the real cause was stigma and major depression that prevented this young adult from seeking or accepting the medical and life saving care that he needed.
Chris Golden was my step-son. His mother and I buried Chris on May 5, 2005. Look at all the ROI numbers, but never forget. This is not about numbers. It’s about people and saving lives. It’s about the Chris Goldens of the world.
Companies can no longer treat stress, depression, or any mental illness as a single diagnosis. Because of coexisting mental illnesses, many employees will not effectively recover from or stabilize chronic and persistent conditions such as diabetes, asthma, heart conditions, hypertension, or cancer unless an effective stress management program is implemented.
A 2005 study for Dupont Company by the University of Pennsylvania showed that depression, when measured by its impact on total costs (direct and indirect costs), was the highest corporate cost medical condition. The second highest total cost was from musculoskeletal issues that likely also involved stress related costs.
See also: Consumerism: Good, Bad, Future
Medical, clinical, and medication therapies have advanced such that clinical depression and other mental health conditions have cure rates equal to and greater than many medical conditions. Clinical depression can be cured. Treatments work. Medications are effective. No company, large or small, can avoid the costs of depression. Divorce, disability, and violence in the workplace can hit anyone at anytime. According to the Institute of Medicine 30,000 people die each year from suicide, and 90% had diagnosable and treatable depression. For a small employer the results can be devastating if a key employee or executive suffers from clinical depression.
Tom Johnson, former CEO of CNN News, likes to say, “If a company’s computers crashed and corporate production ground to a halt, the CEO would demand immediate action to re-establish the “corporate brains.” In developing a “knowledge-based” workforce, it is just as important for CEOs to take care of mental health and the “central computer” – the brain - within each employee.”
Most employers do not understand the complexities of clinical mental health diagnoses. They do not know what it means to have schizophrenia, a somatoform disorder, a factitious disorder, or get a multi-axial assessment. Tom Johnson understood as he often suffered from serious bouts of clinical depression. Tom has dedicated his life to helping others deal with the debilitating effects of depression.
Case Study
As an actuary and mathematician, I was trained in numbers and actuarial science. Many of you may also be analysts, doctors, lawyers, CEOs, economists, or researchers. Let’s throw away the numbers for a moment and look at the lives of real people.
Let me tell you about a young man, age 30, who suffered multiple inherited physical problems: a blood disorder, clotting concerns, pulmonary hypertension, and other unfathomable sources of pain and suffering. Combined with depression and the stigma of an emotional disorder, this young man was frequently non-compliant with care and treatment. Unlike other physical illnesses, depression typically causes the patient to avoid care. He pushed away the very help that was needed. He pushed away family support and friends that cared.
No young strapping 6’5” 260 pound young man wants his forehead stamped with the stigma of mental illness. He was not going to be classified as “crazy”, see a “shrink”, or go to a “nut house” for care. No, he was a high school basketball star with the athletic promise most boys just dream about. In his mind, he didn’t need care, he was who he was. He didn’t accept or understand chemical imbalances. In his mind, "Real men are strong enough."
In 2005 the years of depression and physical decline took its toll. The death certificate read pulmonary hypertension. But, I can tell you the real cause was stigma and major depression that prevented this young adult from seeking or accepting the medical and life saving care that he needed.
Chris Golden was my step-son. His mother and I buried Chris on May 5, 2005. Look at all the ROI numbers, but never forget. This is not about numbers. It’s about people and saving lives. It’s about the Chris Goldens of the world.






