The 2014 WC Benchmarking Study by Rising Medical Solutions depicts a claims industry with nowhere to hide and a lot to answer for. This very detailed and intelligent survey deserves some serious attention.
The survey is particularly revealing because it boldly juxtaposes four critical topics rather than focus on a single issue. The covered topics are:
- Core competencies
- Talent development and retention
- Impact of technology and data
- Medical performance and management
Surveying these four topics together prevents industry excuses. By contrast, any single-topic survey leaves the industry with room to equivocate and retort with presumptuous hope about the holistic system. For example, a survey on talent management might conclude that there is a woeful lack of investment in recruiting and training new adjusters, yet the editorial response might assert that efforts in work-flow technology can take up future slack. Further, a single-topic study showing a higher cost for WC medicine vs. non-occupational care might evoke an editorial response touting the latest strides in "managed care" that surely hold hope for future corrections to this problem.
Well, when a side-by-side evaluation of the four survey topics show consistent deficits in all areas among more than 400 responders I don't think there is enough fresh coffee in any PR department to conjure up a reassuring response.
High-level findings include:
- Claim providers can easily cite the critical core competencies for adjusters: return to work, medical management and compensability investigations, etc. However, many do not measure performance based on these competencies, nor support active efforts to develop these talents. Only half of responders report using positive or negative reinforcement of core competencies.
- Regarding adjuster training, 48% of responders have no or "unknown" budgets. Only 36% have formal training for new hires, most of which is 40 hours or less.
- Fewer than 40% of responders use outcome-based claim measures.
- Fewer than 30% measure medical provider performance, indicating that the network discount is all important and that the care itself an afterthought.
- The IT/data areas indicate no clear focus or vision or investment in workflow, cross-system integration or predictive modeling. (Only 25% report using predictive analytics. Being a proud skeptic of this folly, that is fine with me, but hold that thought for a future article.)
There is creative cross-referencing one can do among this survey's sections, which I believe shows responders' disregard for outcome in favor of profit. For example, one section measures the use of cost-containment applications, while a separate section asks for ranking of cost-containment applications based on how critical they are. Nurse triage is listed as having the third most critical impact on outcome yet is in 7th place among tactics responders use. In contrast, bill review is number one in use, by 95% of responders, yet ranks as only 6th on scale of impact on outcome.
I conclude that, in spite of bill review's low impact on outcomes, many claim-service providers deem the "percentage of savings" cash flow stream as most important. Let's not forget there is a huge IT investment in bill scanning and processing centers. So, despite pressure on other aspects of IT, there apparently is an IT budget available when it supports cash flow.
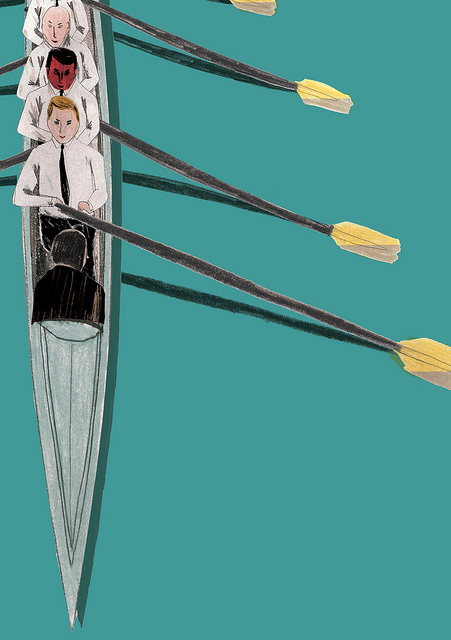
Bottom line, claim providers do little to invest in long-term improvement, while focusing on short-term savings and cash-flow streams.
My suggestion for future studies by Rising Medical is to totally split for-profit insurers and TPAs from in-house, self-administered responders. The former chases profit; the latter chases outcomes. I predict a very telling dichotomy among this split.