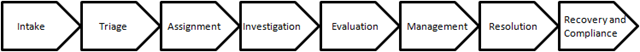
 Which creates an intriguing possibility for an insurance company -- an alternative to bricks and mortar and company cars and salaries, a virtual claims operation! Of course, there are third-party administrators (TPAs) that are large and well-developed enough to offer complete, end-to-end claims management and fulfillment services to an insurance company through an outsourced arrangement. That would be the one-stop shopping solution: hiring a TPA to replace your claims operation. But try to envision an end-to-end process in which you invite vendors/partners/service providers to compete to handle each component in your claims value chain (including processing handoffs to each other.) You select the best, negotiate attractive rates, lock in service guarantees and manage the whole process simply by monitoring a performance dashboard that displays real time data on effectiveness, efficiency, data quality, regulatory compliance and customer satisfaction.
You would need a system to integrate the inputs from the different suppliers to feed the dashboard, and you would also need to make certain the suppliers all worked together well enough to provide the ultimate customer with a seamless, pain free experience, but you are probably already doing some of that if you use vendors. You would still want to do quality and compliance and leakage audits, of course, but you could always hire a different vendor to do that for you or keep a small team to do it yourself.
Your unallocated loss adjustment expenses (ULAE) would become variable, tied directly to claim volume, and your main operating challenge would be to manage your supply/value chain to produce the most desirable cost and experience outcomes. Improved cycle time, efficiency, effectiveness, data accuracy and the quality of the customer experience would be your value propositions. You could even monitor the dashboard from your beach house or boat -- no more staff meetings, performance reviews, training sessions -- and intervene only when needed in response to pre-defined operational exceptions.
Sounds like a no-brainer. Insurance companies have been outsourcing portions of their value chain to vendors for years, so why haven’t they made their claims operations virtual?
If you are running an insurance company claims operation, you probably know why. Many (probably most) claims executives are proud of and comfortable with their claims operations just the way they are. They believe they are performing their value chain processes more effectively than anyone else could, or that their processes are “core” (so critical or so closely related to their value proposition they cannot be performed by anyone else) and thus sacrosanct, or that they have already achieved an optimal balance between in-house and outsourced services so they don’t need to push it any further. Others don’t like the loss of control associated with outsourcing, or they don’t want to consider disruptive change. Still others think it might be worth exploring, but they don’t believe they can make a successful business case for the investment in systems and change costs. Unfortunately, this may help explain why claims executives are often accused of being stubbornly change averse and overly comfortable with the status quo, but I think it is a bit more complicated than that -- it all begins with the figurative “goggles” we use to self-evaluate claims operations.
If you are running a claims operation, you have an entire collection of evaluation goggles -- the more claims experience you have, the larger your collection. When you have your “experience” goggles on, you compare your operation to others you have read about, or seen in prior jobs, or at competitors, to make sure your activities and results benchmark well and that you are staying up to date with best practices. At least once a year, someone outside of claims probably demands that you put your “budget” goggles on o look for opportunities to reduce ULAE costs. or legal costs, or fines and penalties, or whatever. You probably look through your “customer satisfaction” goggles quite a bit, particularly when complaints are up, or you are getting bad press because of your CAT response, or a satisfaction survey has come out and you don’t look good. Your “stakeholder” goggles help you assess how successful you have been at identifying those who have a vested interest in how well you perform, determining what it is they need from you to succeed, and delivering it. You use your “legal and regulatory compliance” goggles to identify problems before they turn into fines, bad publicity or litigation, much as you use your “no surprises” goggles to continually scan for operational breakdowns that might cause reputational or financial pain, finger pointing and second guessing. Then there are the goggles for “management” -- litigation, disability, medical, vendor -- and for “fraud mitigation” and “recovery” and “employee engagement.” Let’s not forget the “efficiency” goggles, which help you assess unit costs and productivity, and the “effectiveness” and “quality control” goggles, which permit you to see whether your processes are producing intended and expected results. And of course your “loss cost management” goggles give you a good read on how well you are managing all three components of your loss cost triangle, i.e., whether you are deploying and incurring the most effective combination of allocated and unallocated expenses to produce the most appropriate level of loss payments.
Are all those goggles necessary? You bet. Claims management involves complex processes and inputs and a convoluted web of variables and dependencies and contingencies. Most claims executives would probably agree it makes sense to regularly evaluate a claims operation from many different angles to get a good read on what’s working well , what isn’t and where there is opportunity for improvement. The multiple perspectives provided by your goggles help you triangulate causes, understand dependencies and impacts and intelligently balance operations to produce the best outcomes. So even if you do have a strong bias that your organization design is world-class, your people are the best and all processes and outcomes are optimal, the evaluation should give you plenty of evidence-based information with which to test that bias and identify enhancement opportunities -- as long as you keep an open mind.
No matter what you do, however, there will always be others in your organization who enjoy evaluating your claims operation, and they usually aren’t encumbered by such an extensive collection of goggles. They may have only one set that is tuned to budget, or customer experience, or compliance, or they may be under the influence of consultants whose expensive goggles are tuned to detect opportunities for large-scale disruptive/destructive process innovation or transformation in your operation. On the basis of that narrow view, they just might conclude that things need to change, that new operating models need to be explored. Whether you agree or disagree, your evidence-based information should be of some value in framing and joining the debate.
Will we ever see virtual claims operations? Sure. There are many specialized claims service providers operating in the marketplace right now that can perform claims value chain processes faster, cheaper and better than many insurance companies can perform them. The technology exists to integrate multiple provider data inputs and create a performance dashboard. And there are a few large insurance company claims organizations pursuing this angle vigorously right now. I fully expect the companies that rethink and retool their claims value chains to take full advantage of integration of supply chain capabilities and begin to generate improved performance metrics and claim outcomes, ultimately creating competitive advantage for themselves. Does that mean it is time for you to rethink your claims value chain? I think the best way to find out is to put on your “innovation” goggles and take a look!
Which creates an intriguing possibility for an insurance company -- an alternative to bricks and mortar and company cars and salaries, a virtual claims operation! Of course, there are third-party administrators (TPAs) that are large and well-developed enough to offer complete, end-to-end claims management and fulfillment services to an insurance company through an outsourced arrangement. That would be the one-stop shopping solution: hiring a TPA to replace your claims operation. But try to envision an end-to-end process in which you invite vendors/partners/service providers to compete to handle each component in your claims value chain (including processing handoffs to each other.) You select the best, negotiate attractive rates, lock in service guarantees and manage the whole process simply by monitoring a performance dashboard that displays real time data on effectiveness, efficiency, data quality, regulatory compliance and customer satisfaction.
You would need a system to integrate the inputs from the different suppliers to feed the dashboard, and you would also need to make certain the suppliers all worked together well enough to provide the ultimate customer with a seamless, pain free experience, but you are probably already doing some of that if you use vendors. You would still want to do quality and compliance and leakage audits, of course, but you could always hire a different vendor to do that for you or keep a small team to do it yourself.
Your unallocated loss adjustment expenses (ULAE) would become variable, tied directly to claim volume, and your main operating challenge would be to manage your supply/value chain to produce the most desirable cost and experience outcomes. Improved cycle time, efficiency, effectiveness, data accuracy and the quality of the customer experience would be your value propositions. You could even monitor the dashboard from your beach house or boat -- no more staff meetings, performance reviews, training sessions -- and intervene only when needed in response to pre-defined operational exceptions.
Sounds like a no-brainer. Insurance companies have been outsourcing portions of their value chain to vendors for years, so why haven’t they made their claims operations virtual?
If you are running an insurance company claims operation, you probably know why. Many (probably most) claims executives are proud of and comfortable with their claims operations just the way they are. They believe they are performing their value chain processes more effectively than anyone else could, or that their processes are “core” (so critical or so closely related to their value proposition they cannot be performed by anyone else) and thus sacrosanct, or that they have already achieved an optimal balance between in-house and outsourced services so they don’t need to push it any further. Others don’t like the loss of control associated with outsourcing, or they don’t want to consider disruptive change. Still others think it might be worth exploring, but they don’t believe they can make a successful business case for the investment in systems and change costs. Unfortunately, this may help explain why claims executives are often accused of being stubbornly change averse and overly comfortable with the status quo, but I think it is a bit more complicated than that -- it all begins with the figurative “goggles” we use to self-evaluate claims operations.
If you are running a claims operation, you have an entire collection of evaluation goggles -- the more claims experience you have, the larger your collection. When you have your “experience” goggles on, you compare your operation to others you have read about, or seen in prior jobs, or at competitors, to make sure your activities and results benchmark well and that you are staying up to date with best practices. At least once a year, someone outside of claims probably demands that you put your “budget” goggles on o look for opportunities to reduce ULAE costs. or legal costs, or fines and penalties, or whatever. You probably look through your “customer satisfaction” goggles quite a bit, particularly when complaints are up, or you are getting bad press because of your CAT response, or a satisfaction survey has come out and you don’t look good. Your “stakeholder” goggles help you assess how successful you have been at identifying those who have a vested interest in how well you perform, determining what it is they need from you to succeed, and delivering it. You use your “legal and regulatory compliance” goggles to identify problems before they turn into fines, bad publicity or litigation, much as you use your “no surprises” goggles to continually scan for operational breakdowns that might cause reputational or financial pain, finger pointing and second guessing. Then there are the goggles for “management” -- litigation, disability, medical, vendor -- and for “fraud mitigation” and “recovery” and “employee engagement.” Let’s not forget the “efficiency” goggles, which help you assess unit costs and productivity, and the “effectiveness” and “quality control” goggles, which permit you to see whether your processes are producing intended and expected results. And of course your “loss cost management” goggles give you a good read on how well you are managing all three components of your loss cost triangle, i.e., whether you are deploying and incurring the most effective combination of allocated and unallocated expenses to produce the most appropriate level of loss payments.
Are all those goggles necessary? You bet. Claims management involves complex processes and inputs and a convoluted web of variables and dependencies and contingencies. Most claims executives would probably agree it makes sense to regularly evaluate a claims operation from many different angles to get a good read on what’s working well , what isn’t and where there is opportunity for improvement. The multiple perspectives provided by your goggles help you triangulate causes, understand dependencies and impacts and intelligently balance operations to produce the best outcomes. So even if you do have a strong bias that your organization design is world-class, your people are the best and all processes and outcomes are optimal, the evaluation should give you plenty of evidence-based information with which to test that bias and identify enhancement opportunities -- as long as you keep an open mind.
No matter what you do, however, there will always be others in your organization who enjoy evaluating your claims operation, and they usually aren’t encumbered by such an extensive collection of goggles. They may have only one set that is tuned to budget, or customer experience, or compliance, or they may be under the influence of consultants whose expensive goggles are tuned to detect opportunities for large-scale disruptive/destructive process innovation or transformation in your operation. On the basis of that narrow view, they just might conclude that things need to change, that new operating models need to be explored. Whether you agree or disagree, your evidence-based information should be of some value in framing and joining the debate.
Will we ever see virtual claims operations? Sure. There are many specialized claims service providers operating in the marketplace right now that can perform claims value chain processes faster, cheaper and better than many insurance companies can perform them. The technology exists to integrate multiple provider data inputs and create a performance dashboard. And there are a few large insurance company claims organizations pursuing this angle vigorously right now. I fully expect the companies that rethink and retool their claims value chains to take full advantage of integration of supply chain capabilities and begin to generate improved performance metrics and claim outcomes, ultimately creating competitive advantage for themselves. Does that mean it is time for you to rethink your claims value chain? I think the best way to find out is to put on your “innovation” goggles and take a look!Rethinking the Claims Value Chain
It is now possible to make the claims process virtual -- and monitor all your vendors from a dashboard in your beach house or on your boat.
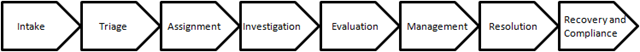 Which creates an intriguing possibility for an insurance company -- an alternative to bricks and mortar and company cars and salaries, a virtual claims operation! Of course, there are third-party administrators (TPAs) that are large and well-developed enough to offer complete, end-to-end claims management and fulfillment services to an insurance company through an outsourced arrangement. That would be the one-stop shopping solution: hiring a TPA to replace your claims operation. But try to envision an end-to-end process in which you invite vendors/partners/service providers to compete to handle each component in your claims value chain (including processing handoffs to each other.) You select the best, negotiate attractive rates, lock in service guarantees and manage the whole process simply by monitoring a performance dashboard that displays real time data on effectiveness, efficiency, data quality, regulatory compliance and customer satisfaction.
You would need a system to integrate the inputs from the different suppliers to feed the dashboard, and you would also need to make certain the suppliers all worked together well enough to provide the ultimate customer with a seamless, pain free experience, but you are probably already doing some of that if you use vendors. You would still want to do quality and compliance and leakage audits, of course, but you could always hire a different vendor to do that for you or keep a small team to do it yourself.
Your unallocated loss adjustment expenses (ULAE) would become variable, tied directly to claim volume, and your main operating challenge would be to manage your supply/value chain to produce the most desirable cost and experience outcomes. Improved cycle time, efficiency, effectiveness, data accuracy and the quality of the customer experience would be your value propositions. You could even monitor the dashboard from your beach house or boat -- no more staff meetings, performance reviews, training sessions -- and intervene only when needed in response to pre-defined operational exceptions.
Sounds like a no-brainer. Insurance companies have been outsourcing portions of their value chain to vendors for years, so why haven’t they made their claims operations virtual?
If you are running an insurance company claims operation, you probably know why. Many (probably most) claims executives are proud of and comfortable with their claims operations just the way they are. They believe they are performing their value chain processes more effectively than anyone else could, or that their processes are “core” (so critical or so closely related to their value proposition they cannot be performed by anyone else) and thus sacrosanct, or that they have already achieved an optimal balance between in-house and outsourced services so they don’t need to push it any further. Others don’t like the loss of control associated with outsourcing, or they don’t want to consider disruptive change. Still others think it might be worth exploring, but they don’t believe they can make a successful business case for the investment in systems and change costs. Unfortunately, this may help explain why claims executives are often accused of being stubbornly change averse and overly comfortable with the status quo, but I think it is a bit more complicated than that -- it all begins with the figurative “goggles” we use to self-evaluate claims operations.
If you are running a claims operation, you have an entire collection of evaluation goggles -- the more claims experience you have, the larger your collection. When you have your “experience” goggles on, you compare your operation to others you have read about, or seen in prior jobs, or at competitors, to make sure your activities and results benchmark well and that you are staying up to date with best practices. At least once a year, someone outside of claims probably demands that you put your “budget” goggles on o look for opportunities to reduce ULAE costs. or legal costs, or fines and penalties, or whatever. You probably look through your “customer satisfaction” goggles quite a bit, particularly when complaints are up, or you are getting bad press because of your CAT response, or a satisfaction survey has come out and you don’t look good. Your “stakeholder” goggles help you assess how successful you have been at identifying those who have a vested interest in how well you perform, determining what it is they need from you to succeed, and delivering it. You use your “legal and regulatory compliance” goggles to identify problems before they turn into fines, bad publicity or litigation, much as you use your “no surprises” goggles to continually scan for operational breakdowns that might cause reputational or financial pain, finger pointing and second guessing. Then there are the goggles for “management” -- litigation, disability, medical, vendor -- and for “fraud mitigation” and “recovery” and “employee engagement.” Let’s not forget the “efficiency” goggles, which help you assess unit costs and productivity, and the “effectiveness” and “quality control” goggles, which permit you to see whether your processes are producing intended and expected results. And of course your “loss cost management” goggles give you a good read on how well you are managing all three components of your loss cost triangle, i.e., whether you are deploying and incurring the most effective combination of allocated and unallocated expenses to produce the most appropriate level of loss payments.
Are all those goggles necessary? You bet. Claims management involves complex processes and inputs and a convoluted web of variables and dependencies and contingencies. Most claims executives would probably agree it makes sense to regularly evaluate a claims operation from many different angles to get a good read on what’s working well , what isn’t and where there is opportunity for improvement. The multiple perspectives provided by your goggles help you triangulate causes, understand dependencies and impacts and intelligently balance operations to produce the best outcomes. So even if you do have a strong bias that your organization design is world-class, your people are the best and all processes and outcomes are optimal, the evaluation should give you plenty of evidence-based information with which to test that bias and identify enhancement opportunities -- as long as you keep an open mind.
No matter what you do, however, there will always be others in your organization who enjoy evaluating your claims operation, and they usually aren’t encumbered by such an extensive collection of goggles. They may have only one set that is tuned to budget, or customer experience, or compliance, or they may be under the influence of consultants whose expensive goggles are tuned to detect opportunities for large-scale disruptive/destructive process innovation or transformation in your operation. On the basis of that narrow view, they just might conclude that things need to change, that new operating models need to be explored. Whether you agree or disagree, your evidence-based information should be of some value in framing and joining the debate.
Will we ever see virtual claims operations? Sure. There are many specialized claims service providers operating in the marketplace right now that can perform claims value chain processes faster, cheaper and better than many insurance companies can perform them. The technology exists to integrate multiple provider data inputs and create a performance dashboard. And there are a few large insurance company claims organizations pursuing this angle vigorously right now. I fully expect the companies that rethink and retool their claims value chains to take full advantage of integration of supply chain capabilities and begin to generate improved performance metrics and claim outcomes, ultimately creating competitive advantage for themselves. Does that mean it is time for you to rethink your claims value chain? I think the best way to find out is to put on your “innovation” goggles and take a look!
Which creates an intriguing possibility for an insurance company -- an alternative to bricks and mortar and company cars and salaries, a virtual claims operation! Of course, there are third-party administrators (TPAs) that are large and well-developed enough to offer complete, end-to-end claims management and fulfillment services to an insurance company through an outsourced arrangement. That would be the one-stop shopping solution: hiring a TPA to replace your claims operation. But try to envision an end-to-end process in which you invite vendors/partners/service providers to compete to handle each component in your claims value chain (including processing handoffs to each other.) You select the best, negotiate attractive rates, lock in service guarantees and manage the whole process simply by monitoring a performance dashboard that displays real time data on effectiveness, efficiency, data quality, regulatory compliance and customer satisfaction.
You would need a system to integrate the inputs from the different suppliers to feed the dashboard, and you would also need to make certain the suppliers all worked together well enough to provide the ultimate customer with a seamless, pain free experience, but you are probably already doing some of that if you use vendors. You would still want to do quality and compliance and leakage audits, of course, but you could always hire a different vendor to do that for you or keep a small team to do it yourself.
Your unallocated loss adjustment expenses (ULAE) would become variable, tied directly to claim volume, and your main operating challenge would be to manage your supply/value chain to produce the most desirable cost and experience outcomes. Improved cycle time, efficiency, effectiveness, data accuracy and the quality of the customer experience would be your value propositions. You could even monitor the dashboard from your beach house or boat -- no more staff meetings, performance reviews, training sessions -- and intervene only when needed in response to pre-defined operational exceptions.
Sounds like a no-brainer. Insurance companies have been outsourcing portions of their value chain to vendors for years, so why haven’t they made their claims operations virtual?
If you are running an insurance company claims operation, you probably know why. Many (probably most) claims executives are proud of and comfortable with their claims operations just the way they are. They believe they are performing their value chain processes more effectively than anyone else could, or that their processes are “core” (so critical or so closely related to their value proposition they cannot be performed by anyone else) and thus sacrosanct, or that they have already achieved an optimal balance between in-house and outsourced services so they don’t need to push it any further. Others don’t like the loss of control associated with outsourcing, or they don’t want to consider disruptive change. Still others think it might be worth exploring, but they don’t believe they can make a successful business case for the investment in systems and change costs. Unfortunately, this may help explain why claims executives are often accused of being stubbornly change averse and overly comfortable with the status quo, but I think it is a bit more complicated than that -- it all begins with the figurative “goggles” we use to self-evaluate claims operations.
If you are running a claims operation, you have an entire collection of evaluation goggles -- the more claims experience you have, the larger your collection. When you have your “experience” goggles on, you compare your operation to others you have read about, or seen in prior jobs, or at competitors, to make sure your activities and results benchmark well and that you are staying up to date with best practices. At least once a year, someone outside of claims probably demands that you put your “budget” goggles on o look for opportunities to reduce ULAE costs. or legal costs, or fines and penalties, or whatever. You probably look through your “customer satisfaction” goggles quite a bit, particularly when complaints are up, or you are getting bad press because of your CAT response, or a satisfaction survey has come out and you don’t look good. Your “stakeholder” goggles help you assess how successful you have been at identifying those who have a vested interest in how well you perform, determining what it is they need from you to succeed, and delivering it. You use your “legal and regulatory compliance” goggles to identify problems before they turn into fines, bad publicity or litigation, much as you use your “no surprises” goggles to continually scan for operational breakdowns that might cause reputational or financial pain, finger pointing and second guessing. Then there are the goggles for “management” -- litigation, disability, medical, vendor -- and for “fraud mitigation” and “recovery” and “employee engagement.” Let’s not forget the “efficiency” goggles, which help you assess unit costs and productivity, and the “effectiveness” and “quality control” goggles, which permit you to see whether your processes are producing intended and expected results. And of course your “loss cost management” goggles give you a good read on how well you are managing all three components of your loss cost triangle, i.e., whether you are deploying and incurring the most effective combination of allocated and unallocated expenses to produce the most appropriate level of loss payments.
Are all those goggles necessary? You bet. Claims management involves complex processes and inputs and a convoluted web of variables and dependencies and contingencies. Most claims executives would probably agree it makes sense to regularly evaluate a claims operation from many different angles to get a good read on what’s working well , what isn’t and where there is opportunity for improvement. The multiple perspectives provided by your goggles help you triangulate causes, understand dependencies and impacts and intelligently balance operations to produce the best outcomes. So even if you do have a strong bias that your organization design is world-class, your people are the best and all processes and outcomes are optimal, the evaluation should give you plenty of evidence-based information with which to test that bias and identify enhancement opportunities -- as long as you keep an open mind.
No matter what you do, however, there will always be others in your organization who enjoy evaluating your claims operation, and they usually aren’t encumbered by such an extensive collection of goggles. They may have only one set that is tuned to budget, or customer experience, or compliance, or they may be under the influence of consultants whose expensive goggles are tuned to detect opportunities for large-scale disruptive/destructive process innovation or transformation in your operation. On the basis of that narrow view, they just might conclude that things need to change, that new operating models need to be explored. Whether you agree or disagree, your evidence-based information should be of some value in framing and joining the debate.
Will we ever see virtual claims operations? Sure. There are many specialized claims service providers operating in the marketplace right now that can perform claims value chain processes faster, cheaper and better than many insurance companies can perform them. The technology exists to integrate multiple provider data inputs and create a performance dashboard. And there are a few large insurance company claims organizations pursuing this angle vigorously right now. I fully expect the companies that rethink and retool their claims value chains to take full advantage of integration of supply chain capabilities and begin to generate improved performance metrics and claim outcomes, ultimately creating competitive advantage for themselves. Does that mean it is time for you to rethink your claims value chain? I think the best way to find out is to put on your “innovation” goggles and take a look!